Can hip abduction reducetherisk of femoral head necrosisdeteriorated into osteoarthritis?A 3D finiteelement analysis
Guang-Quan Zhou,Hong-Lai Zhang
1 The First Affiliated Hospital,Guangzhou University of Chinese Medicine,Guangzhou,China.2 School of Medical Information Engineering,Guangzhou University of Chinese Medicine,Guangzhou,China.
Background
Femoral head necrosis(FHN)is a pathological process,with the characteristics of initially injury of necrotic bone trabecular structure that occurs in the load-bearing zone of the femoral head and the subsequent repair process of the injured bone tissue.As the damage-repair process continues,it results in structural changes of the femoral head,collapse and deformation,and finally osteoarthritis(OA)and joint dysfunction.In the theroy of traditional Chinese medicine(TCM),FHN is called Gushi,which was first recorded in Huangdineijing published on Xihan Dynasty of China(the third century B.C.).
FHN is a debilitating disease which generally affects young adults,resulting in femoral head collapse and OA.In Asia,there is approximately 40%of the primary hip replacement caused by OA after FHN[1].In addition to drug therapy,the conventional conservative management methodshaveinvolved restricted weight-bearing,bed rest,surgery and traction therapy.However,weight-bearing and bed rest may result in osteoporosis,slow metabolism,muscle atrophy and poor clinical curative effect[2,3].Several hip preserving surgery methods[4-9]have been developed to interrupt the disease pathway of collapse and OA after FHN,averting the need for hip replacement.Isolated core decompression will accelerate a collapse and OA progression of the femoral head because of the lack of repaired materials and biomechanical structural support during the healing of the necrosis region[10,11].Free vascularized fibular grafting can provide immediate structural support and vascularity,but it is often associated with serious trauma,technical difficulties and longer recovery time. Transtrochanetric rotational osteotomy[7]can improve the biomechanical properties in daily activity and effectively decreased the average stress by either anterior or posterior rotation.However,it is a technically demanding procedure associated with high complication risks.
Clinical doctors and researchers share a common goal of choosing safe and effective treatment procedure for protecting the femoral head of the patients with FHN[12,13].Non-drug therapy is the commonly therapeutic method in the field of TCM rehabilitation therapy,including rest,reasonable exercise and joint function exercise.Lower extremity abduction(LEA)represents an effective hip preservation method in TCM rehabilitation therapy,which can relieve pain,eliminate inflammation and preserve the shape of the femoral head without surgery intervention,restricted weight-bearing and bed rest.Enhanced LEA motion is associated with a decrease in postnecrotic OA.This therapy works help to move the necrotic portion away from the weight-bearing area to reduce stress concentration,improve the biomechanical properties via full weight-bearing in daily activity[14],enhance the ability of bony healing via increasing stress stimulation[15,16],and decrease the peak contact hip stress[17].However,these conclusions are mainly based on observational clinical experience,which makes it controversial.
Clinical practice concept requires proof in theory.We postulated that the enhanced LEA motion during gait may reduce the risk of collapse of FHN via reconstructing the stress transfer patterns and protect against OA progression.To test this hypothesis,thirty parametric computational models were generated to investigate biomechanical behavior changes of FHN by increasing the lower extremity abducent angle,offering scientific basis on choosing the proper treatment for the exact classification.
Material and methods
Japanese Investigation Committee(JIC)classification
In 2001,the JIC revised diagnostic criteria to clarify the definition of osteonecrosis of the femoral head[18,19].According to the JIC classification criteria,FHN can be classified into subtypes A,B,C1 and C2,based on the location of the lesion in the weight-bearing area(as shown in Figure 1).Type A lesions occupy the medial one-third or less of the weight-bearing portion,while type B lesions occupy the medial two-thirds or less of the weight-bearing portion.Type C1 lesions occupy more than the medial two thirds of the weight-bearing portion without extending laterally to the acetabular edge.Type C2 lesions occupy more than the medial two-thirds of the weight-bearing portion and extend laterally to the acebtabular edge.
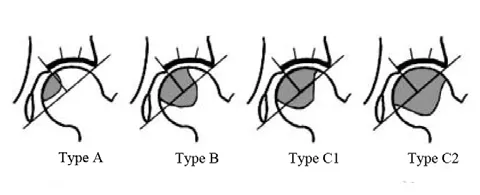
Figure 1 JIC classification of FHN[18]
Parametric modeling
Five computational models were generated as a healthy model and four subtype models of FHN based on JIC classification criterion.The parametric definition of the models enabled the study of the effect of abduction on stress transfer.Single-legged stance was considered as a representative body position for the primary models.We used an abducent angle β (β =0°,10°,15°,20°,25°and 30°)as a variable[20,21]along the anteroposterior axis of femoral head to investigate stress transfer path(STP)and contact stress.The abducent variants were depicted schematically in Figure 2.Finally,a total of thirty different computational models were used to simulate six hip abductions with fivedifferent progresses of FHN.
Boundary conditions
A ground reaction force equivalent to body weight was exerted on a rigid plate that tied to the distal femur.Constrains were applied to pubic symphysis and sacroiliac joint.All six degrees of freedom were constrained to zero for all cases described above.Seven muscles were modeled as axial connectors and muscle forces were depicted in literature[22].In this study,the muscleforceswere postulated to be constantsduring LEA gait.The parametric finite element analysis was performed using ABAQUSV6.13.All models were input to generate isotropic 10-node tetrahedral elements.The mesh sizewas3 mm.
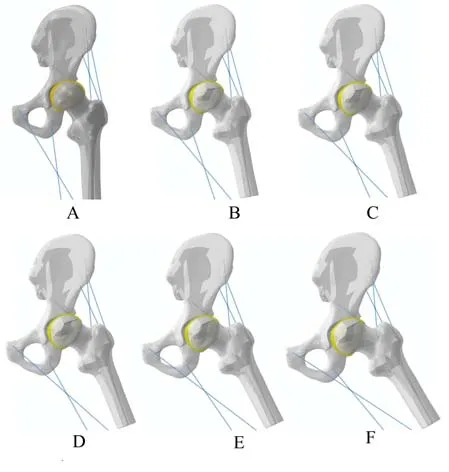
Figure2 Lower extremity abducent angle
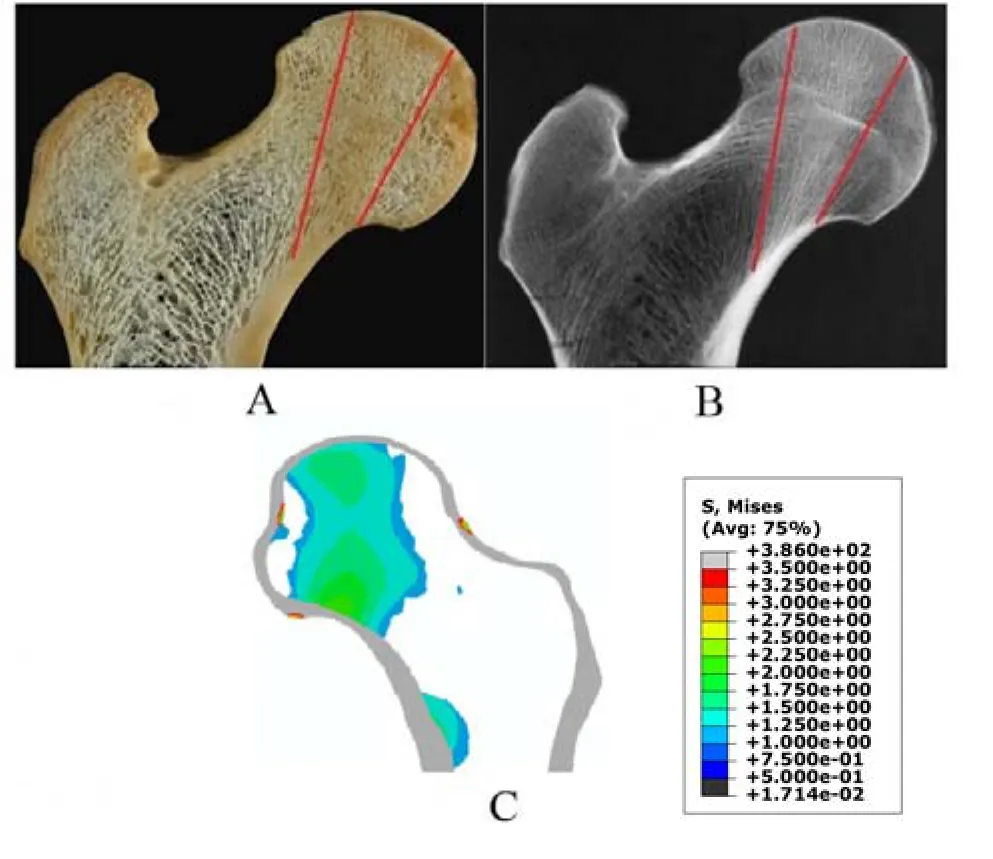
Figure 3 Photograph,radiograph and computational results of human proximal femur
Model validation
The model validation of this study was performed by comparing the median coronal femoral head nephogram and the median coronal femoral trabecular bone profile of normal subjects.
Results
Model validation
The major function of principal compressivetrabeculae in the proximal femur is loading principal stress.The stress trabecula carries the conduction of principal stress,and the direction of conduction is from femur head bearing area to femoral moment(Figure 3C),which correlates well with the trabecular features in the cross-sections of the cadaver bone(Figure 3A)and the bone density distribution(Figure 3B)[27-29].These phenomenons conform to Wolff’s law:the structure and function of bone are interdependent[30].Hence,the biomechanical behavior of this model was considered valid.
Stress transfer path
In this study,STPis the measurable change of load borne in femoral head during LEA motion.The effects of stress transfer characteristics were evaluated and the coronal contours of proximal femur on stress were plotted.As shown in the Figure 4,on normal conditions the STPs moved from weight-bearing region to lateral column with increasing LEA angles;on stance conditions(β=0°)the STP of type A(Figure 4B)showed strong similarities with the healthy level(Figure 4A);STP distribution was from the top of the femoral head to the calcar;the damage area of STP of type B(Figure 4C)was approximately 25%of the healthy condition.While STPs in both type C1 and C2(Figure 4D and Figure 4E)were broken off.The damage areas of STPof type C were more than 50%of the healthy condition.As the increase of the abduction angle,STPs of the femoral head were increasing restoration;type B could be transformed into type A,while type C1 could be transformed into type B;type C2 could be transformed into type C1.
Contact stress
Contact stress is an important biomechanical index in evaluation of OA progression between pre-treatment and post-treatment[23,24].Since elevated contact stress may accelerate the progression of OA,the peak values and average values of the contact stress were used for the analysis.The contact pattern varied according to the simulated loading activity.Figure 5 show the relationship between the LEA motion and the likelihood of OA progression.Greater LEA motion would increase the peak contact stress underlying healthy condition,which is in accordance with previous literature[25,26].However,in this study,there was no significant difference in peak contact stress between the four settings of FHN and normal femoral head.The average values of the contact stress in four setting lay within the range of values corresponding to normal setting.
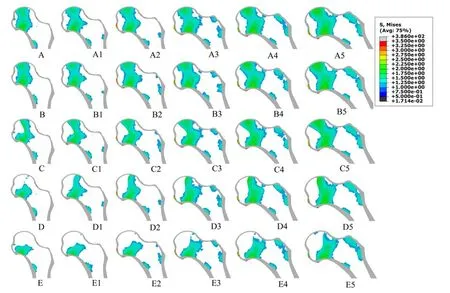
Figure4 Stresstransfer path
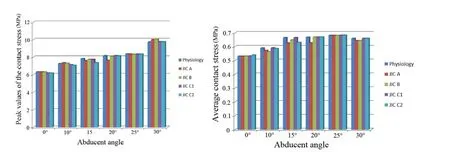
Figure5 Thecontact stressof articular cartilage
Discussion
In recent years,various hip preserve methods have been developed to maintain the femoral head of the patients and reconstruct the biomechanical stability to prevent the FHN deteriorated into OA in the pre-collapse stage.In some way,these procedures delay or interrupt the likelihood of hip replacement.Hence,femoral head preservation methods still play an important role in the management of FHN.Enhanced LEA motion is an effective femoral head preservation method,which could stop the progression of FHN without reducing weight-bearing and bed rest and surgery intervention.Enhanced LEA motion improves the biomechanical properties of bone density and muscle force as well as speeds up the metabolism during cyclic loadings in daily activity.However,the best classification for LEA intervention and itsmechanism are still unclear.
Computational biomechanical approach has the potential to quantify the relationship between hip morphology,cartilage mechanics and OA[31,32].Computational techniques can make the scientific experiments feasible,which could provide biomechanical basis for understanding the mechanisms of hip and the degeneration progression of FHN without requiring in vivo studies.Evidence suggests that mechanical factors play an important role in the development and progression of OA[33,34].Hip joint is the largest enarthrosis joint of human;its pathological progression is closely related to the biomechanics[35].Hence,in this study, we adopted computational biomechanical techniques to investigate the effect of enhanced LEA motion on OA progression after FHN.
The purpose of this study was to investigate biomechanical behavior changes of necrotic femoral head during increasing LEA angle,offering scientific basis on choosing the LEA procedure for the exact classifications.In this study,thirty computational biomechanical models were used and the results indicated that the deterioration of FHN into OA is dependent on the extent of STP recovery.We hypothesized that enhanced LEA motions during gait may recover the STP of femoral head and protect against OA progression.The results of this study support our hypothesis:Firstly,as shown in Figure 4,LEA motions could adjust the STPof the femoral head in all conditions.As increasing the LEA angle,STPof type B could be transformed into type A,STPof type C1 could be transformed into type B.STP of type C2 could be transformed into type C1.The lower classification is associated with the lower risk of collapse.Hence,we believe that enhanced LEA motions could reduce the collapse risk of FHN,especially during type A,B and C1,while type C2 of FHN involved surgical intervention may get a better clinical outcome.STP loads principal compressive stress,whose morphology may reflect the function of principal compressive trabeculae.Damage areas of STP gradually reduce in all classifications of FHN as increasing LEA motions.Hence,we believe that enhanced LEA motions may recover the bearing capability of trabeculae.These may due to the reason that the LEA motions moved the principal compressive stress from necrotic region to lateral normal trabeculae.As a result,the cortical bones need not to overload with work to retain the morphology and function of the femoral head.Second,Hadley and Maxian reported that the excessive hip joint contact stress may contribute to the processes of OA[36,37];in our study,as shown in Figure 5,the results reveal that there was no significant difference in contact stress between the four settings of FHN and normal femoral head during LEA motions.These findings provided unique biomechanical insight into treatment results of LEA motion in FHN.Hence,we believed that enhanced LEA motions could not increase the risk of OA.
Conclusion
In summary,the results from our computational biomechanical analysis suggest that enhanced LEA motion can effectively reduce collapse risk and interrupt the disease pathway of FHN deteriorated into OA in the early stages of FHN.Furthermore,our findings indicate that the LEA procedure is suitable for type A,B and C1,while type C2 of FHN involved surgical intervention may get abetter clinical outcome.
1. Lai YS,Wei HW,Cheng CK.An analysis of hip replacement data of Taiwan.The Northern Region Congress of the Asia Pacific Orthopaedic Association in Conjunction with the Third Annual Meeting of the Pacific Asian Society of Minimally Invasive Spine Surgery Taipei,Taiwan 2003:5-6.
2. Stephen JI,Charles NP.Diagnosis and classification of avascular necrosis of the hip.Semin Arthroplasty 2004,15:140-144.
3. Michael JG. Resurfacing arthroplasty in osteonecrosisof the hip.Orthop Clin NAm 2005,36:231-242.
4. Petrigliano FA,Lieberman JR.Osteonecrosis of the hip:novel approaches to evaluation and treatment.Clin Orthop 2007,465:53-62.
5. Korompilias AV,Lykissas MG,Beris AE,et al.Vascularised fibular graft in the management of femoral head osteonecrosis:twenty years later.J Bone Joint Surg 2009,9:287-293.
6. Sugioka Y,Yamamoto T.Transtrochanteric posterior rotational osteotomy for osteonecrosis.Clin Orthop 2008,466:1104-1109.
7. Mel SL,Tai CL,Senan V,et al.The effect of necrotic lesion and rotational degree on the stress reduction in transtrochanteric rotational osteotomy for femoral head osteonecrosis:a three dimensional finite element simulation.Clin Biomech 2006,21:969-976.
8. Urbaniak JR,Congan PG,Gunneson JA.Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting:a long term follow-up study of one hundred and three hips.J Bone Joint Surg 1995,77:6881-6894.
9. Wang BL,Sun ZC,Zhang NF,et al.Treatment of nontraumatic osteonecrosis of the femoral head using bone impaction grafting through a femoral neck window.Int Orthop 2010,34:635-639.
10.Camp JF,Colwell CW.Core decompression of the femoral head for osteonecrosis.J Bone Joint Sugr 1986,68:1313-1319.
11.Koo KH,Kim R,Ko GH,et al.Preventing collapse in early osteonecrosis of the femoral head,a randomized clinical of core decompression.J Bone joint Sugr 1995,77:870-874.
12.Hasegawa Y,Iwata H,Torii S,et al.Vascularized pedicle bone-grafting for nontraumatic avascular necrosis of the femoral head:a 5-to 11-year follow up.Arch Orthop Trauma Surg 1997,116:251-258.
13.Krachow KA,Mont MA,Maar DC.Limited femoral endoprosthesis for avascular necrosis of the femoral head.Orthop Rev 1993,22:457-463.
14.Cui YF,Yuan H.A clinical study of Yuan’s plastic therapy for treatment of osteonecrosis of femoral head.Fam Med Community Health 2005,21:1760-1762.
15.He W,Yuan H,Fang B,et al.A study on repairing mechanism of the femoral head necrosis treated with Chineseherb.JMed biomech 2000,15:162-165.
16.Zhang YF,Zhang YX.Mechanical factorsof femoral head necrosis after operation of femoral head neck fracture.JBone Joint Injury 2001,16:270-272.
17.Dolinar D,Kralj-Iglic V.Influence of contact hip stress on the outcome of surgical treatment of hips affected by avascular necrosis.Arch Orthop Trauma Surg 2003,123:509-513.
18.Sugano N,Atsumi T,Ohzono K,et al.The 2001 revised criteria for diagnosis,classification,and staging of idiopathic osteonecrosis of the femoral head.JOrthop Sci2002,7:601-605.
19.Sugano N,Kubo T,Takaoka K,et al.Diagnostic criteria for non-traumatic osteonecrosis of the femoral head:a multicenter study.JBone Joint Sugr 1999,81:590-595.
20.Zhang MC,Shi FL,Zhao WD,et al.Stress distribution on the femoral head neck at different abduction angles of the hip joint:a finite element analysis.JFirst Mil Med Univ 2005,25:1244-1246.
21.Tian FD,Zhao DW,Guo L,et al.Influence of step width and abduction angle on necrotic femur head by three-dimensional finite element method.Chinese journal of tissue engineering research 2012,16:3052-3055.
22.Sverdlova SN,Witzel U.Principles of determination and verification of muscle forces in the human musculoskeletal system:muscle force to minimize bending stress.JBiomech 2010,43:387-396.
23.Brand RA,Iglic A,Kralj-Iglic V.Contact stress in the human hip:implications for disease and treatment.Hip Int 2001,11:117-126.
24.Pauwels F.Biomechanics of the normal and diseased hip 1976.Springer Berlin Heidelberg,New York.
25.David EK,Leonard E,Patrick OR,et al.Exercise and gait effects on in vivo hip contact pressures.Phys Ther 1991,71:301-309.
26.Hak DH,Hamel AJ,Bay BK,et al.Consequences of transverse acetabular fracture malreduction on load transmission across the hip joint.J Orthop Trauma 1998,12:90-100.
27.Jang IG,Kim IY.Computation simulation of trabecular adaptation progress in human proximal femur during growth.JBiomech 2009,42:573-580.
28.Boyle C,Kim IY.Three-dimensional micro-level computational study of Wolff’s law via trabecular bone remodeling in the human proximal femur using design space topology optimization.JBiomech 2011,44:935-942.
29.Jang IG,Kim IY.Computational study of Wolff’s law with trabecular architecture in the human proximal femur using topology optimization.J Biomech 2008,41:2353-1361.
30.Wolff J. The law of bone Remodeling.Springer-Verlag,Berlin Heidelberg New York,1986(translation of the german 1892 edition).
31.Von Eisenhart-Rothe RAC, Steinlechner M,Muller-Gerbl M,et al.Quantitative determination of joint incongruity and pressuer distribution during simulated gait and cartilage thickness in the human hip joint.JOrthop Res 1999,7:532-539.
32.Genda E,Konishi N,Hasegawa Y,et al.A computer simulation study of normal and abnormal hip joint contact pressure.Arch Orthop Trauma Surg 1995,114:202-206.
33.Mankin HJ,The reaction of articular cartilage to injury and osteoarthritis(first of two parts).N Engl J Med 1974,291:1285-1292.
34.Mankin HJ.The reaction of articular cartilage to injury and osteoarthritis(second of two parts).N Engl JMed 1974,291:1335-1340.
35.Harrison MHM, Schajowicz F, Trueta J.Osteoarthritis of the hip:A study of the nature and evolution of the disease.Bone Joint J 1953,35:598-626.
36.Hadley N,Brown T,Weinstein S.The effects of contact stress pressure eleveations and aseptic necrosis in the long-term outcome of congenital hip dislocation.JOrthop Res1990,8:504-513.
37.Maxian TA,Brown TD,Weinstein SL.Chronic stress tolerance levels for human articular cartilage:Two nonumiform contact models applied to long term follow-up of CDH.J Biomechanics 1995,28:159-166.
 Traditional Medicine Research2018年5期
Traditional Medicine Research2018年5期
- Traditional Medicine Research的其它文章
- Theconcept of vaccinesfirst came from Chinesemedicine
- Rat model for study of the essence of spleen deficiency and dampness in Chinese medicine
- Evaluating theclinical efficacy of Thunder-Firemoxibustion combined with ovulation monitoring in thetreatment of adenomyosiscombined with infertility
- Clinical efficacy of combined skin acupuncture and external washing therapy of Zhuang nationality medicine in the treatment of chronic eczema
- Bioactive molecules in Siddha Polyherbal Nilavembu Kudineer alleviating symptoms of Dengue/Chikugunya
- Is Thunder-Fire moxibustion effective in the treatment of adenomyosis combined with infertility?
