Out of hospital cardiac arrest resuscitation outcome in North India — CARO study
Chennappa Kalvatala Krishna, Hakim Irfan Showkat, Meenakshi Taktani, Vikram Khatri Department of Cardiology, Moolchand Medcity, New Delhi, India
2 Department of Cardiology, National Heart Institute, New Delhi, India
Out of hospital cardiac arrest resuscitation outcome in North India — CARO study
Chennappa Kalvatala Krishna1, Hakim Irfan Showkat2, Meenakshi Taktani1, Vikram Khatri11Department of Cardiology, Moolchand Medcity, New Delhi, India
2Department of Cardiology, National Heart Institute, New Delhi, India
BACKGROUND: To evaluate the outcome of cardiopulmonary resuscitation (CPR) in out-ofhospital cardiac arrests (OHCA) in India and factors inf l uencing the outcome.
METHODS: The outcome and related factors like demographics, aspects of the OHCA event,return of spontaneous circulation (ROSC) and survival to discharge, among the 80 adult patients presenting to emergency department experiencing OHCA considered for resuscitation between January 2014 to April 2015, were analyzed, according to the guidelines of the Utstein consensus conference.
RESULTS: The survival rate to hospital admission was 32.5%, the survival rate to hospital discharge was 8.8% and with good cerebral performance category (CPC1) neurological status was 3.8%. Majority of OHCA was seen in elderly individuals between 51 to 60 years, predominately in males. Majority of OHCA were witnessed arrests (56.5%) with 1.3% bystander CPR rate, 92.5% arrests occurred at home, 96% presented with initial non-shockable rhythm and 92.5% with presumed cardiac etiology but survival was better in those who experienced OHCA at public place, in witnessed arrests, in patients who had shockable presenting rhythm and in those where CPR duration was ≤20 minutes.
CONCLUSION: Witnessed arrests, early initiation of CPR by bystanders, CPR duration ≤20 minutes, initial presenting shockable rhythm, OHCA with non-cardiac etiology are associated with a good outcome. To improve the outcome of CPR and the low survival rates after an OHCA event in India, focused strategies should be designed to set up an emergency medical system (EMS), to boost the rates of bystander CPR and education of the lay public in basic CPR.
Out-of-hospital cardiac arrest; Cardiopulmonary resuscitation; Survival to discharge; Shockable rhythm; Bystander CPR; Witnessed arrest; CPR duration; Cardiac etiology
INTRODUCTION
Out of hospital cardiac arrest (OHCA) is one of the leading cause of death in India. There are very few studies in India, on the outcome after cardiopulmonary resuscitation (CPR) in patients with OHCA. However, due to lack of pre-medical emergency service system (EMS),lack of EMS protocols, limited medical resources and equipment, inadequate infrastructure, lack of emergency medical personnel training, lack of knowledge and skills of CPR among bystanders and in the community; the outcome of OHCA in India will be poor, as compared to western countries, where EMS systems are an integral part of the health care system, which routinely provides CPR to every victim of cardiac arrest (CA).[1]
So the ultimate goal of this study is to collect data on outcome of CPR in patients with OHCA, factors influencing the outcome and to identify the strong predictors of these outcomes, which is the need of the hour, to help administrators and medical directors,identify the changes to be made to optimize system interventions and improve CA outcomes. Since this study focuses on outcome of resuscitation in cardiac arrests,so it has been coined as Cardiac Arrest Resuscitation Outcome (CARO) study.
METHODS
This study was conducted at Department of Emergency Medicine of a multispecialty urban hospitals;well equipped with 24–hour state of the art Emergency Facilities with Ambulance Services & Intensive care units.With institutional approval, all adult patients above the age of 18 years, who suffered out-of-hospital cardiac arrests(OHCA) between January 2014 to April 2015, were taken in this study. A total of 80 cardiac arrests were identif i ed.
Exclusion criteria
Patients under the age of 18 years or with obvious signs of death (e.g., rigor mortis or dependent lividity)or experiencing CA in the hospital setting were excluded from the study.
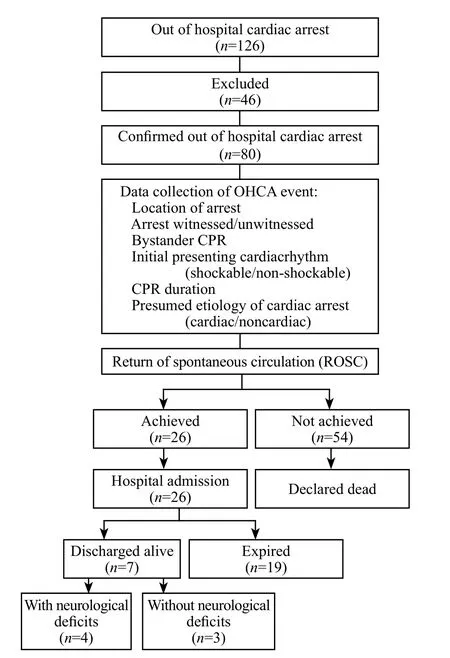
Figure 1. Flow chart of study design.
Using a CPR Performa and the flow chart given below, information was collected on (Figure 1): (1)age, sex, co-morbid conditions and location of CA; (2)whether the arrest was witnessed or not; (3) who initiated CPR (bystander); (4) initial presenting cardiac rhythm(shockable or non-shockable); (5) whether there was a return of spontaneous circulation (ROSC); (6) probable etiology of CA; (7) whether the patient survived to discharge; (8) whether the patient was discharged with or without any neurological def i cits.
Data collection
All the data from patients were analysed according to the guidelines of the Utstein consensus conference(Utstein-style definitions).[2]
Out of hospital cardiac arrest (OHCA)
An OHCA was defined as cessation of cardiac mechanical activity, conf i rmed by the absence of signs of circulation (no central pulsation, unresponsiveness, and apnea or agonal, gasping respirations)[3]and that occurs outside of a hospital setting
Location of arrest
Location of arrest was the specific location where the event occurred or the patient was found: place of residence (e.g., home, apartment, back yard of a home);public place (e.g., street, city park, shopping center,sports stadium, entertainment center, airport, railway station, church); others (e.g., hotel room, private off i ce).
Bystander CPR
Bystander CPR was CPR performed by a person who is not responding as part of an organized emergency response system approach to a cardiac arrest. Physicians,nurses, and paramedics may be described as performing bystander CPR if they are not part of the emergency response system involved in the victim's resuscitation.
First monitored rhythm
The first monitored rhythm was the first cardiac rhythm present when a monitor is attached to a patient after CA.
Shockable/non-shockable rhythm
Shockable/non-shockable rhythm was referred to the first monitored rhythm, which when analyzed by the person interpreting the monitor was found to be treatable by attempted defibrillation (i.e., shockable or non-shockable). In general, shockable CA rhythms were further divided into ventricular fi brillation and pulseless ventricular tachycardia. Non-shockable CA rhythms was categorized as either asystole or pulseless electrical activity (PEA).
Return of spontaneous circulation (ROSC)
ROSC was intended to represent a brief (approximately>30 seconds) restoration of spontaneous circulation that provides evidence of more than an occasional gasp,occasional fleeting palpable pulse, or arterial waveform.
End of event
A resuscitation event is deemed to have ended when death is declared or spontaneous circulation is restored and sustained for 20 minutes or longer.
Survived event to hospital admission
"Survived event" for the OHCA means sustained ROSC with spontaneous circulation until admission and transfer of care to the ICU staff.
Cause of arrest (etiology)
A probable etiology of CA was judged by analyzing the circumstances leading to the event and the patient's past medical history. An arrest was presumed to be of cardiac etiology unless it is known or likely to have been caused by trauma, submersion, drug overdose, asphyxia,exsanguination, or any other non-cardiac cause as best determined by rescuers.
Date of discharge/death
The date of discharge or death was the date on which the patient was discharged from the hospital or was certified dead.
Neurological outcome at discharge from hospital
A simple validated neurological score such as the Cerebral Performance Category (CPC)[3]was recorded.CPC was assessed at hospital discharge. (1) CPC 1. Good cerebral performance. Conscious, alert, able to work;might have mild neurologic or psychological deficit.(2) CPC 2. Moderate cerebral disability. Conscious,sufficient cerebral function for independent activities of daily life. Able to work in sheltered environment. (3)CPC 3. Severe cerebral disability. Conscious, dependent on others for daily support because of impaired brain function. Ranges from ambulatory state to severe dementia or paralysis. (4) CPC 4. Coma or vegetative state. Any degree of coma without the presence of all brain death criteria. Unawareness, even if appears awake (vegetative state) without interaction with environment; might have spontaneous eye opening and sleep/awake cycles.
RESULTS
Baseline characteristics
Eighty patients suffering from OHCA were identif i ed in this study. Patient's demographics and aspects of the OHCA events are given below (Table 1). The mean age of the 80 patients who suffered OHCA was 63±14.6 years. The population was predominantly composed of elderly individuals with highest percentage of OHCA seen between 51 to 60 years. About 70% of the patients were males and 30% were females (P<0.001).
Aspects of the OHCA event
Out of 80 patients, 74 (92.5%) experienced OHCA at residence and only 6 (8.1%) had OHCA at other locations (P<0.001) (Table1). Totally 46 (56.5%) of OHCA were witnessed, out of which 15.2% patients survived; whereas 42.5% were unwitnessed, of which none of them survived (P=0.017). Although 46 (56.5%)of OHCA events were witnessed by a bystander, only 1 (1.3%) of these arrests received bystander CPR(P<0.001). Three (3.8%) of study population presented with initial shockable rhythm (VF/pulseless VT) and out of which 2 (66.6%) survived; 5 (6.4%) patients survivedout of 77 (96.3%) patients who presented with initial non-shockable (asystole/PEA) rhythm (P<0.001). CPR duration of 30 minutes was taken as a cut off and it was found that of 47 (59%) of patients with OHCA, who received CPR for a duration of less than or equal to 30 minutes, ROSC was achieved in 32.5% of them whereas not a single patient could be revived in the remaining 26(32.5%) of patients, who received CPR for a duration of more than 30 minutes (P=0.013). The majority of cardiac arrests were of presumed cardiac etiology (74, 92.5%),of which only 6.7% survived. Six (7.5%) of OHCA were of non-cardiac etiologies, of which 33.3% survived(P=0.02).
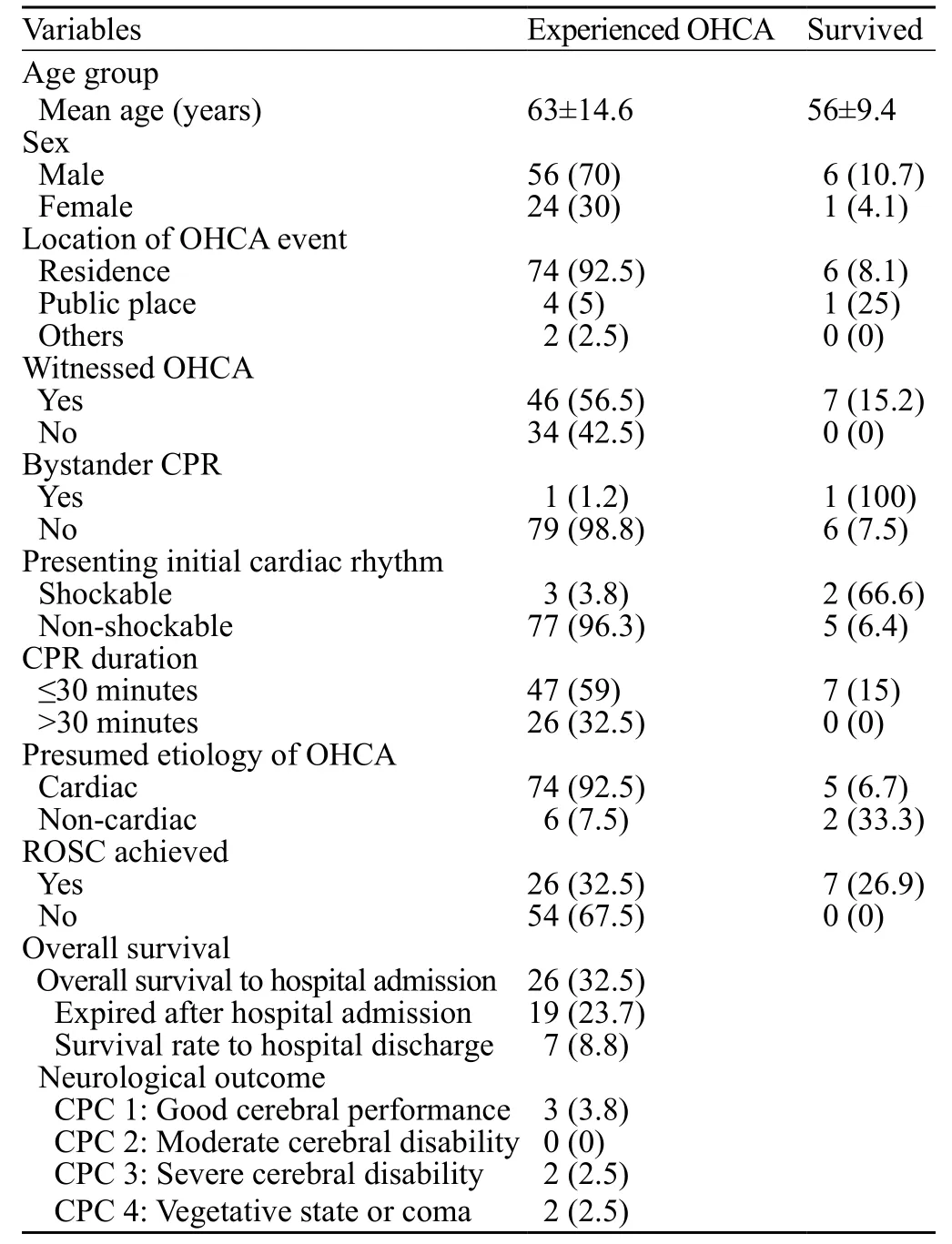
Table 1. Patient's demographics and aspects of the OHCA events, n (%)
Outcomes
Overall, successful resuscitation (ROSC) was achieved in 26 (32.5%) patients, however only 7 (8.8%)were discharged alive from the hospital and the rest 19(23.7%) expired after hospital admission (Table 1). Out of the 7 patients discharged alive (P<0.001), 3 (3.8%) were discharged with good cerebral performance, 2 (2.5%) were discharged with severe cerebral disability and the rest 2(2.5%) were discharged in vegetative comatose state.
Predictors of outcome: univariate and multivariate analysis
Univariate analysis of the data examined the effect of the predictor variables on alive at discharge (Table 2).We compared predictors like age <60 years, male sex,initial presenting rhythm, CPR duration of ≤20 minutes,non-cardiac etiology with likelihood of being alive at discharge. We found that presenting shockable cardiac rhythm (=0.01), CPR duration of ≤20 minutes (=0.002), the arrest with non-cardiac etiology (=0.049),were significantly associated with likelihood of being alive at discharge.
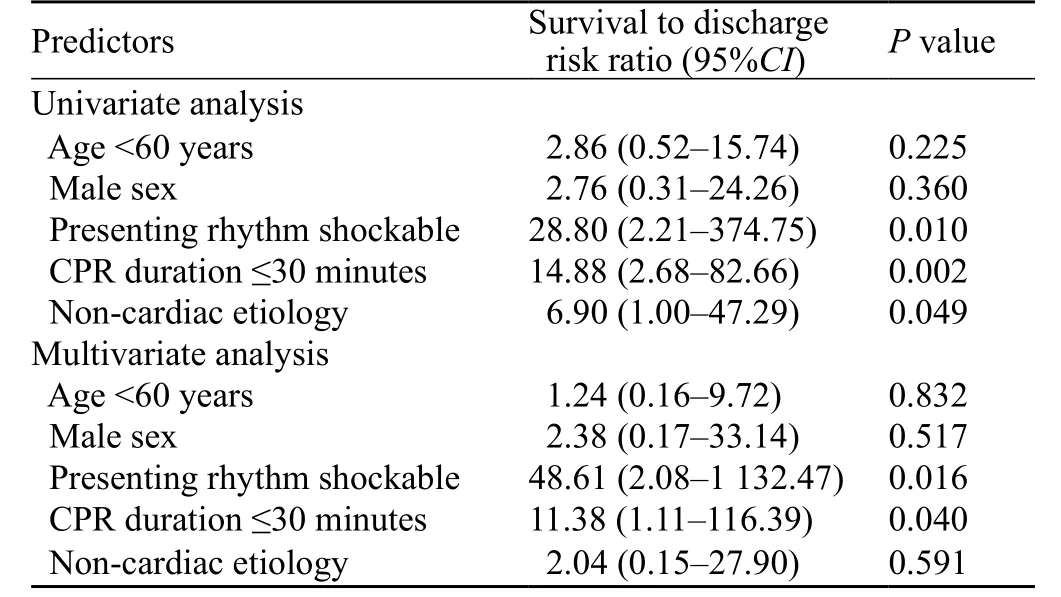
Table 2. Predictors of outcome after CPR (univariate & multivariate analysis)
Independent predictors of alive at the time of discharge from the hospital were CPR duration of ≤20 minutes (=0.04) and presenting shockable rhythm (=0.016) (Table 2). Bystander CPR and witnessed arrest were important factors influencing on the outcome of CPR in OHCA, these variables could not be introduced into the univariate and multivariate models, probably due to small sample size.
DISCUSSION
In India, there have been very limited data on the outcome of cardiopulmonary resuscitation in out-ofhospital cardiac arrests. Our study has shown that the survival rate to hospital admission was 32.5%, and the overall survival rate to hospital discharge was 8.8%and survival to hospital discharge with good cerebral performance was 3.8%. This fi gure is slightly higher than in certain previous reports, like an Indian study published in 1999 by Rajaram et al,[4]which showed the overall survival rate to hospital discharge was 5.9%. If we compare with western countries, where BLS and ACLS protocols and emergency medical services (EMS) are well developed; the overall survival to hospital discharge rate is 9.6% (CARES),[5]so we are still lagging behind.
One of the major cause of low survival rates for an OHCA event is due to lack of EMS which is an essential part of the overall healthcare system.[6]Despite tremendous development in the healthcare sector, India is yet to create a single, comprehensive EMS that can be accessed throughout the country; which explains the cause of no significant change in the survival rates for past many decades. In a bid to address this problem, the Centralized Accidents and Trauma Services were set up by the Indian Government in the early 1990s. Inspite of having a centralized number "102" and a nationwide expansion, it failed to gain the acceptance equal to western EMS.[6,7]Moreover, there are no set EMS protocols to follow with regard to patient assessment,triage, transfer and disposition to a medical facility for ambulance or emergency medical personnel.
Low survival rates after an OHCA event are of great public health concern. So to avoid preventable deaths and disabilities, there is an urgent need of a centralized medical emergency body which could provide guidelines for setting up emergency services and should be involved in preparing protocols, imparting technical assistant,training and accreditation of emergency services.[7]
Our study also evaluated specific factors associated with survival after OHCA, including age, sex, arrest witnessed by a bystander, bystander CPR, presenting cardiac rhythm, duration of CPR and etiology of arrest.
According to the study results, highest percentage of OHCA was predominantly seen in elderly individuals between 51 to 60 years (33.8%). Advanced age has been shown to be a predictor of poor survival after CPR,[3,8,9]but in our study though increasing age was negatively associated with survival, but it was not statistically significant. OHCA was more common in males (70%)as compared to females (=0.003). International studies[4,10]showed that 61.1% to 70.1% were males who experienced OHCA where as Indian study by Rajaram et al showed 66% males. These data do suggest that males are more prone for OHCA than females; but regarding relationship between survival after OHCA and sex of the individual, it was statistically non-significant; further studies with large number of samples in this context are required.
Our study showed that 74 (92.5%) patients out of 80 had OHCA at home out of which 6 (8.1%) survived,whereas four (5%) individuals arrested at public place among whom one received bystander CPR and survived.International data suggested that OHCA at residence were less likely to be witnessed and have poorer outcome,[10]likewise in our study too, OHCA at home was associated with poor survival outcome as compared to public place.
CPR outcomes were better in witnessed arrests;57.5% patients had a witnessed OHCA, out of which 15.2% patients survived (<0.01), but no single patient survived from the remaining 42.5% unwitnessed arrests.EMS witnessed OHCA have not been considered for comparison from these studies because of lack of a good EMS service in India.
Studies[11,12]have shown that bystander CPR is associated with good outcome in OHCA with a significant improvement in survival and alive at discharge as compared with the no bystander CPR.In our study, although 56.5% of OHCA events were witnessed by a bystander, only 1 (1.3%) of these arrests received bystander CPR (<0.001). This is very poor in comparison to the 18%–55% rates reported from the West.[13]Such a low frequency of bystander CPR is one of the major cause of low survival rates after an OHCA event. Unfortunately in India, bystander CPR rates have remained very low, due to lack of awareness of basic CPR techniques among the communities.[13]Improving community bystander CPR rates is an important step towards improving OHCA survival. There is an urgent need of national initiatives to strengthen bystander resuscitation attempts and advanced care by educational campaigns (e.g., brief educational videos, community awareness programs),[14,15]and implementing schoolbased training.[16]
The duration of CPR is a good predictor of outcome as demonstrated by us and numerous others.[17–19]In our study, CPR duration of 30 minutes was taken as a cut off and it was found that out of 59% patients with OHCA, who received CPR for a duration of less than or equal to 30 minutes, ROSC was achieved in 32.5%of them whereas not a single patient could be revived in the remaining 32.5% of patients, who received CPR for a duration of more than 30 minutes. This shows that the CPR duration of more than 30 minutes in OHCA patients is associated with very poor outcome. An important consideration in outcome prediction in OHCA is the time of collapse until definitive resuscitation intervention begun. However, we were unable to collect correct information as the reported time of CR was often what was recalled by a friend or family member and was likely to be erroneous especially in unwitnessed CR.
Majority of the patients (96%) presented with nonshockable rhythm, whereas only 3 (3.8%) patients presented with initial shockable cardiac rhythm (VT/VF),but patients who had initial shockable presenting rhythm were observed to have better survival (<0.001). These results were identical to the results of earlier studies,[20,21]which described, survival to hospital discharge was substantially more likely when the first documented rhythm was shockable rather than non-shockable.
Our study also demonstrated that in majority of the OHCA, the etiology was found to be cardiac in origin(92.5%), but good survival outcome was seen in OHCA with non-cardiac etiology (<0.001). Univariate analysis of the data also showed that OHCA with non-cardiac etiology is the one important predictor of survival to discharge after CPR in OHCA.
CONCLUSION
The present data suggest that witnessed arrests,early initiation of CPR by bystanders, CPR duration≤20 minutes, initial presenting shockable rhythm,OHCA with non-cardiac etiology are associated with good outcome after CPR in OHCA. Age and sex did not influence the outcome. To improve the outcome of CPR and the low survival rates after an OHCA event in India, focused strategies should be designed to create a centralized medical emergency body which could provide guidelines for setting up emergency medical system (EMS), preparing emergency protocols, imparting technical assistant and training. There is also an urgent need of a national initiative to boost the rates of bystander CPR and education of the lay public in basic CPR, which is very critical to improve the survival of OHCA events.
ACKNOWLEDGMENTS
This research was supported/partially supported by Moolchand Medcity, New Delhi, India. We take this opportunity to express our gratitude to all of the Emergency Department fellow colleagues for their help and support. We thank all our colleagues who provided insight and expertise that greatly assisted the research.
Funding: This research was partially supported supported by Moolchand Medcity, New Delhi, India.
Ethical approval: This work is approved by the Institutional Review Board.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.Contributors: Krishna CK proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
1 Rao KS. Background Papers of the National Commission on Macroeconomics and Health. New Delhi: Ministry of Health and Family Welfare, Government of India; 2005. Delivery of health services in the public sector. Financing and Delivery of Health care Services in India; p. 47.
2 Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa).Circulation. 2004;110(21):3385–97.
3 Taffet GE, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. JAMA. 1988;260(14):2069–72.
4 Rajaram R, Rajagopalan RE, Pai M, Mahendran S. Survival after cardiopulmonary resuscitation in an urban Indian hospital, Natl Med J India. 1999;12(2):51–5.
5 McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, et al. Out-of-hospital cardiac arrest surveillance — Cardiac Arrest Registry to Enhance Survival (CARES), United States,October 1, 2005— December 31, 2010. MMWR Surveill Summ.2011;60(8):1–19.
6 Subhan I, Jain A. Emergency care in India: the building blocks.Int J Emerg Med. 2010;3(4):207–11.
7 Potluri P. Emergency services in India- Counting on betterment.A transition in progress. Editorial Section. [Last assessed on 2011 Jan 25]; Asian Hospital and health care Management magazine. 2009 18 Available from: http: //www.asianhhm.com /healthcare management/emergency_services_india.htm.
8 Tunstall-Pedoe H, Bailey L, Chamberlain DA, Marsden AK,Ward ME, Zideman DA. Survey of 3 765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. BMJ. 1992;304(6838):1347–51.
9 Schneider AP 2nd, Nelson DJ, Brown DD. In-hospital cardiopulmonary resuscitation: A 30-year review. J Am Board Fam Pract 1993;6(2):91–101.
10 B?ttiger BW, Grabner C, Bauer H, Bode C, Weber T, Motsch J, et al. Long-term outcome after out-of-hospital cardiac arrest with physician staffed emergency medical services: the Utstein style applied to a midsized urban/suburban area. Heart.1999;82(6):674–9.
11 Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM,Christensen EF, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310(13):1377–84.
12 Ritter G, Wolfe RA, Goldstein S, Landis JR, Vasu CM, Acheson A, et al. The effect of bystander CPR on survival of out-ofhospital cardiac arrest victims. Am Heart J. 1985;110(5):932–7.
13 Ballew KA. Cardiopulmonary resuscitation. BMJ.1997;314(7092):1462–5.
14 Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD, et al. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation.2008;117(16):2162–7.
15 Abella BS, Aufderheide TP, Eigel B, Hickey RW, Longstreth WT Jr, Nadkarni V, et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation.2008;117(5):704–9.
16 Nambiar M, Nedungalaparambil NM, Aslesh OP. IIs current training in basic and advanced cardiac life support (BLS &ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala.World J Emerg Med.2016;7(4):263–9.
17 Saklayen M, Liss H, Markert R. In-hospital cardiopulmonary resuscitation. Survival in one hospital and literature review.Medicine (Baltimore). 1995;74(4):163–75.
18 Beer RJ, Teasdale TS, Ghusn HF, Taffet GE. Estimation of severity of illness with APACHE II: Age-related implications in cardiac arrest outcomes. Resuscitation. 1994;27(3):189–95.
19 Lerner EB, Persse D, Souders CM, Sterz F, Malzer R, Lozano M Jr, et al. Design of the Circulation Improving Resuscitation Care(CIRC) Trial: a new state of the art design for out-of-hospital cardiac arrest research. Resuscitation. 2011;82(3):294–9.
20 Kajino K, Iwami T, Daya M, Nishiuchi T, Hayashi Y, Ikeuchi H, et al. Subsequent ventricular fibrillation and survival in outof-hospital cardiac arrests presenting with PEA or asystole.Resuscitation. 2008;79(1):34–40.
21 Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR,Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38(1):101–8.
Accepted after revision April 20, 2017
Hakim Irfan Showkat, Email: docirfanshahi512@gmail.com
World J Emerg Med 2017;8(3):200–205
10.5847/wjem.j.1920–8642.2017.03.007
November 16, 2016
 World journal of emergency medicine2017年3期
World journal of emergency medicine2017年3期
- World journal of emergency medicine的其它文章
- A case of exercise induced rhabdomyolysis from calf raises
- Instructions for Authors
- Iatrogenic Horner's syndrome: A cause for diagnostic confusion in the emergency department
- Ocular mutilation: A case of bilateral self-evisceration in a patient with acute psychosis
- Blunt injury to the thyroid gland: A case of delayed surgical emergency
- Validation of different pediatric triage systems in the emergency department
