Implication of ultrasound bladder parameters on treatment response in patients with benign prostatic hyperplasia under medical management
Rajeev Thekumpadam Puthenveetil*,Debajit Baishya, Sasanka Barua,Debanga Sarma
Department of Urology,Gauhati Medical College Hospital,Guwahati,Assam,India
Implication of ultrasound bladder parameters on treatment response in patients with benign prostatic hyperplasia under medical management
Rajeev Thekumpadam Puthenveetil*,Debajit Baishya, Sasanka Barua,Debanga Sarma
Department of Urology,Gauhati Medical College Hospital,Guwahati,Assam,India
Benign prostatic hyperplasia;
Objective:The prevalence of benign prostatic hyperplasia(BPH)rapidly increases after the 4th decade of life.The combination of tamsulosin and dutasteride is a well established therapy for BPH of≥40 g.Non-invasive urodynamic parameters can predict the outcome of medical therapy in patients with BPH.We aimed to correlate these parameters with treatment responses in BPH patients under medical management.
Methods:A prospective study was conducted in the Department of Urology in our hospital from May 2014 to April 2015.A total of 100 patients with BPH≥40 g who fulfilled our inclusion criteria were included.Treatment responses were determined by the International Prostate Symptom Score(IPSS)and uroflowmetry.Transabdominal ultrasonography with Doppler was performed to measure prostate volume,intravesical prostatic protrusion(IPP),detrusor wall thickness(DWT),the prostatic capsular artery resistive index(RI)and prostatic urethral angle (PUA)before and 3 months after combination therapy of tamsulosin and dutasteride.Treatment responses were correlated with non-invasive urodynamic parameters.
Results:The IPSS,uroflow,age,prostate volume,RI,IPP,DWT and PUA were correlated before and after treatment.Of the 100 patients,70(70%)showed significant improvement and 30 (30%)showed no improvement with therapy.
Conclusion:Ultrasound bladder parameters are useful tools for measuring the treatment response in BPH patients.Our study shows that RI and DWT significantly correlate with the treatment response in BPH patients.More importantly,pretreatment values of increased IPP and PUA determines the non-improvement of symptoms in BPH patients.Our study suggests the importance of transabdominal ultrasonography(KUB-P)with Doppler for evaluating treatment responses to medical management.
?2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier (Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
The prevalence of benign prostatic hyperplasia(BPH)increases rapidly after the 4th decade of life,reaching nearly 100%in the 9th decade[1].The American Urological Association(AUA)symptom score index is widely used and is validated as an important means of assessing men with lower urinary tract symptoms(LUTS)[1].The original AUA symptom score is based on answers to seven questions concerning frequency,nocturia,a weak urinary stream, hesitancy,intermittency,incomplete bladder emptying, and urgency.The International Prostate Symptom Score (IPSS)includes these seven questions,as well as a global quality-of-life question.The total symptom score ranges from 0 to 35,with scores of 0-7,8-19,and 20-35,indicating mild,moderate,and severe LUTS,respectively.The IPSS is a helpful tool for the clinical management of men with LUTS and in research studies regarding medical and surgical treatment of men with voiding dysfunction due to BPH.Uroflowmetry is recommended by the AUA during evaluation of a patient with BPH.Uroflowmetry is the best non-invasive urodynamic test to detect lower urinary tract obstruction[2].The combination of tamsulosin and dutasteride is a well established therapy for BPH greater than 40 g.Non-invasive urodynamic parameters such as intravesical prostatic protrusion(IPP),detrusor wall thickness (DWT),the prostatic capsular artery resistive index(RI)and prostatic urethral angle(PUA)can predict the outcome of medical therapy in patients with BPH.This study is aimed to correlate these non-invasive urodynamic parameters with treatment responses in patients with BPH under medical management.
2.Materials and methods
We conducted a prospective study in the Department of Urology in our hospital from May 2014 to April 2015. Informed consent was taken from the subjects.The inclusion criteria of the patients were an IPSS>15,prostate weight≥40 g,uroflowmetry<15 mL/s,serum prostate specific antigen(PSA)levels<4 ng/mL.Exclusion criteria were other causes of LUTS,such as neurogenic bladder, stricture urethra,urinary tract infection,serum PSA levels>4 ng/mL,prostate weight<40 g and serum creatinine>1.5 mg/dL.A total of 103 patients with BPH greater than 40 g who fulfilled our inclusion criteria were included in the study.A thorough clinical evaluation and laboratory and radiological investigations were performed in all of the patients.Of the 103 patients,three patients were lost to follow up and were excluded from the study.
Treatment responses were determined by the IPSS and uroflowmetry.Transabdominal ultrasonography(KUB-P) with Doppler was performed to measure the prostate weight,prostatic capsular artery RI,DWT,PUA and IPP at the time of starting the combination therapy.The RI of the capsular artery of the prostate was calculated as(peak systolic velocity-end diastolic velocity)/peak systolic velocity,measured by ultrasound Doppler(Fig.1).A cut-off value of 0.69 was considered abnormal in our study population.DWT was the thickness of the hypoechoic muscle between two hyperechoic layers corresponding to the serosa and mucosa.Three measurements of the anterior bladder wall were taken at a filling volume of 250 mL and the average of these was used to measure the DWT(Fig.2). A cut-off value of more than 2.9 mm was considered abnormal in our study population.The PUA was the angle formed by the proximal prostatic urethra with the distal prostatic urethra in sagital section of ultrasonography at a bladder volume of 250 mL(Fig.3).Patients with a PUA≥35°were considered abnormal.IPP was measured by the length from the tip of the protruding prostate into the bladder,to the bladder circumference at the base of the prostate (Fig.4).A cut-off value of more than 5 mm was considered abnormal in our study population.
Combination therapy with tamsulosin 0.4 mg and dutasteride 0.5 mg daily was started in all of the patients for three months.After 3 months of combination therapy, we repeated KUB-P with Doppler to measure the abovementioned parameters.Treatment responses that were determined by the IPSS and uroflowmetry were correlated with the non-invasive urodynamic parameters.Correlation of the prognostic variables was analyzed with the Z-test. p<0.05 was considered significant.
3.Results
The total numbers of patients in our study was 100.Their age ranged 58-70 years with a mean age of 63.5±6.0 years.The prostate weight ranged 41-57 g with a mean weight of 51.2±5.0 g.The uroflow of patients ranged 7-11 mL/s with a mean uroflow of 8.6±2.0 mL/s.The IPSS of the patients ranged 16-24 with a mean IPSS of 20±4. Table 1 shows the mean values of RI,IPP,DW and PUA determined by KUB-P.
Patients were put on combination therapy with tamsulosin(0.4 mg)and dutasteride(0.5 mg)daily for 3 months. The IPSS score and uroflowmetry were done in all patients after 3 months to measure the treatment response.Transabdominal ultrasonography was done to measure prostate volume,RI,IPP,DWT and PUA.
Out of 100 patients,70(70%)patients significantly symptomatically improved(p<0.0001)and 30(30%)patients did not improve with 3 months of combination therapy.The mean values of uroflow and IPSS of these 70 patients were significantly improved after treatment (p<0.0001).The mean values of RI and DWT of these 70 patients were significantly different after treatment compared with that of before treatment(p<0.0001 and p=0.0256).However,mean values of IPP and PUA of these 70 patients were not significantly different after treatment in compared with that of before treatment (p>0.9999)(Table 2).
The mean value of uroflow and IPSS of the 30 patients who did not symptomatically improved were not signif icantly different after treatment which were compared with before treatment(p=0.862 and p=0.832).The mean values of RI,IPP,DWT and PUA of these 30 patients were also not significantly different after treatment compared with before treatment(p=0.17,p>0.999,p=0.9785 and p>0.9999,respectively)(Table 2).
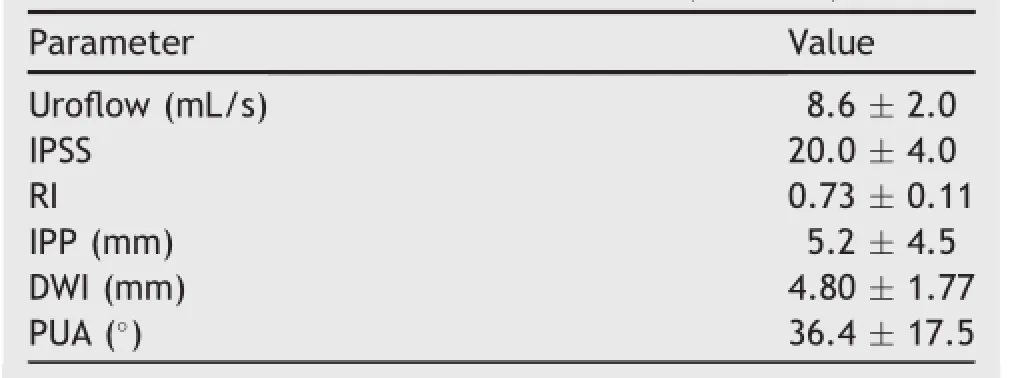
Table 1Parameters before treatment(n=100).
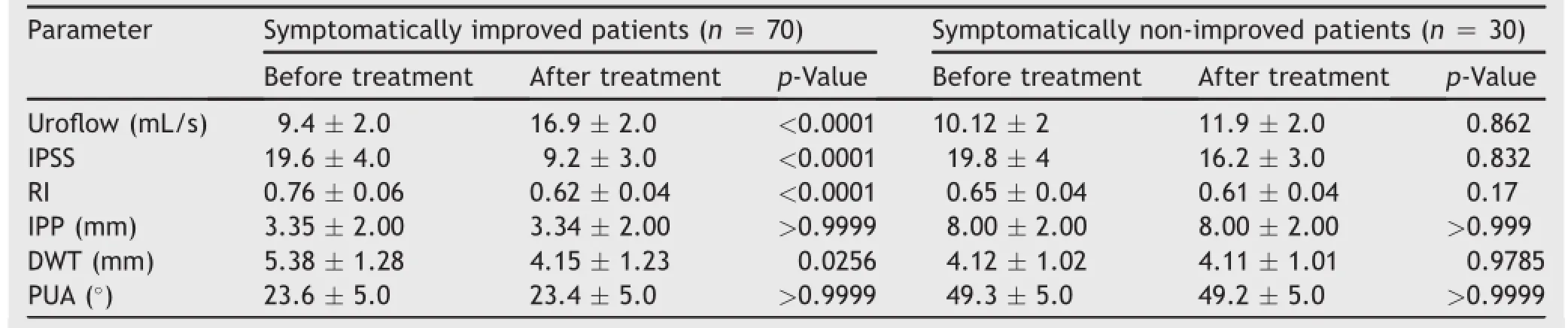
Table 2Parameters in symptomatically improved patients and symptomatically non-improved patients.
The prostate weight of symptomatically improved patients was not significantly different after treatment in compare with before treatment(52.0±4.5 g vs. 52.1±3.2 g,p>0.05).The prostate weight of symptomatically non-improved patients was also not signif icantly different after treatment compared with before treatment(50.0±4.3 g vs.50.1±3.5 g,p>0.05).
4.Discussion
The prevalence of BPH is age dependent[3].BPH usually begins to develop after the age of 40 years,and its prevalence becomes greater than 50%by 60 years,and as high as 100%by 85 years[3].Despite the high prevalence of BPH, its pathogenesis is still poorly understood.
BPH is bothersome to patients when it is combined with LUTS.Urodynamic studies are helpful for assessing men with bothersome LUTS due to BPH.However,the invasive nature of urodynamic studies and potential complications have limited its routine clinical application[4,5].Several recent studies have reported the importance of anatomical factors in evaluating LUTS due to BPH.Transabdominal ultrasonography is a non-invasive study that can be used on an outpatient basis to evaluate the anatomical structure of the prostate.
With the advent of power Doppler imaging,the RI of capsular arteries in patients with LUTS has become a promising parameter in the evaluation of BPH.The definite mechanism through which the RI is elevated in BPH is still unclear[6].Hyperplastic prostate tissue is thought to push the capsule out as it grows,thus increasing the intraprostatic pressure,as well as the RI.A lower IPSS and peakflow rate are correlated with a high RI of capsular arteries. Kojima et al.[7]showed a significant correlation between the RI and urodynamic parameters obtained in peak flow rate(Qmax)of uroflowmetry and IPSS in their study.Shinbo et al.[8]studied the RI as a risk for acute urinary retention in patients with BPH.They found that the RI was increased in patients with BPH and was related to the severity of bladder outlet obstructive symptoms.Kojima et al.[7] also demonstrated that the RI value of patients with a normal prostate volume was significantly lower than that of patients with an enlarged prostate(0.64±0.04 vs. 0.72±0.06;p<0.0001).They found a cut-off value of 0.69,the RI distinguished patients with and without bladder outlet obstruction with 78%sensitivity and 86.4% specificity.In the current study,the mean values of the IPSS and RI in the 70 improved patients decreased.We also found that the uroflow improved after treatment compared with before treatment.These findings clearly indicated that the prostatic capsular artery RI is signif icantly higher in patients with bladder outlet obstruction due to BPH.Additionally,improvement of the RI of capsular arteries directly correlated with improvement of the IPSS and uroflow in patients.Therefore,RI can be used as an index for measurement of improvement in symptoms in lower urinary tract obstruction due to BPH.
Measurement of DWT(thickness of the hypoechoic muscle between two hyperechoic layers corresponding to the serosa and mucosa)by ultrasound is reliable,where at least three measurements of the anterior bladder wall are taken at a filling volume of 250 mL.Using a cut-off value>2.9 mm in men,DWT is considered the best diagnostic tool to measure detrusor hypertrophy[9].In symptomatically improved patients after 3 months of combination therapy, the IPPS was improved,DWT was reduced and uroflow was increased compared with before treatment.In patients with no symptomatic improvement,after 3 months of therapy,the IPPS,uroflow and DWT were not significantly different compared with before treatment.These findings suggest that a decrease in DWT significantly correlated with an improvement in the IPSS.
The prostatic urethra is a bent tube,and the clinical significance of the PUA was recently reported[10,11].An increased PUA may be the result of a higher bladder neck in men who have no lateral or median prostatic lobe enlargement[11].Although some urologists suspect that a higher bladder neck might be due to the presence of BPH, the clinical significance of PUA is not well understood.The prostatic urethra runs through the prostate from the base to the apex,making an anterior angle of 35°at the proximal part of the verumontanum.This bend divides the urethra into the proximal and distal portions[12].By applying fluid dynamics to the process of urination in the prostatic urethra,Cho et al.[11]suggested that energy loss in the bending tube in the prostatic urethra could occur during micturition.They insisted that because of the increased energy loss resulting from the PUA,this leads to a decrease in urine velocity,and the urine flow rate is inversely associated with the PUA[10].Ku et al.[13]found that as the PUA increases,the bladder outlet obstruction index increases.Patients with a PUA≥35°were more likely to haveoutlet obstruction than those with PUA<35°.In our study, in 70 patients who symptomatically improved after combination therapy as mentioned above,the IPSS improved, while uroflow was increased after treatment but there was little change in the PUA.However,in the 30 patients who did not improve symptomatically,the mean values of the IPSS,uroflow and PUA were unchanged after treatment compared with before treatment.These results indicated that pretreatment values of a large PUA were significantly correlated with non-improvement of symptoms in patients with BPH.
IPP is a morphological change by which the prostate protrudes into the bladder during the process of prostatic enlargement.It is induced by enlargement of the median lobe,which leads to a ball-valve type of bladder outlet obstruction.As a result,there is abnormal movement of the bladder leading to inhibition of the funnel effect of the bladder neck at urination[14,15].Chia et al.[16]described that strong bladder contractions open the channel between the lateral lobes,but accelerate the ball-valve effect by IPP.This induces more bladder outlet obstruction than with enlargement of the lateral lobe alone without IPP.In our study,in 70 patients who symptomatically improved after combination therapy while IPSS improved and uroflow increased after treatment,there was little change in IPP. However,in the 30 patients who did not improve symptomatically,the mean values of the IPSS,uroflow and PUA were unchanged after treatment compared with before treatment.These results showed that a higher pretreatment IPP was significantly correlated with no improvement of symptoms in patients with BPH.
5.Conclusion
Ultrasound bladder parameters,such as IPP,DWT,the RI, and the PUA are considered as potential non-invasive clinical tools for baseline assessment of patients with bladder outlet obstruction.Our study shows that the RI and DWT are significantly correlated with the treatment response in patients with BPH.More importantly,pretreatment values of high IPP and PUA do not affect a lack of improvement in symptoms in patients with BPH.This preliminary prospective study indicates that ultrasound bladder parameters are useful tools for measuring the treatment response in patients with BPH.A long-term study with a large series is required to con firm our findings.
Conflicts of interest
The authors declare no conflict of interest.
[1]Barry MJ,Fowler Jr FJ,O’Leary MP,Bruskewitz RC, Holtgrewe HL,Mebust WK,et al.The American Urological Association symptom index for benign prostatic hyperplasia.J Urol 1992;148:1549-57.
[2]McConnell JD,Barry MJ,Bruskewitz RC.Benign prostatic hyperplasia:diagnosis and treatment.Clinical practice guideline No.8.Rockville,MD:U.S.Department of Health and Human Services,Agency for Health Care Policy and Research,Public Health Service;1994.p.1-17.
[3]Berry SJ,Coffey DS,Walsh PC,Ewing LL.The development of human benign prostatic hyperplasia with age.J Urol 1984;132: 474-9.
[4]Klingler HC,Madersbacher S,Djavan B,Schatzl G, Marberger M,Schmidbauer CP.Morbidity of the evaluation of the lower urinary tract with transurethral multichannel pressure-flow studies.J Urol 1998;159:191-4.
[5]Onur R,Ozden M,Orhan I,Kalkan A,Semercioz A.Incidence of bacteraemia after urodynamic study.J Hosp Infect 2004;57: 241-4.
[6]Ozdemir H,Onur R,Bozgeyik Z,Orhan I,Ogras MS,Ogur E. Measuring resistance index in patients with BPH and lower urinary tract symptoms.J Clin Ultrasound 2005;33:176-80.
[7]Kojima M,Ochiai A,Naya Y,Okihara K,Ukimura O,Miki T. Doppler resistive index in benign prostatic hyperplasia:correlation with ultrasonic appearance of the prostate and infravesical obstruction.Eur Urol 2000;37:436-42.
[8]Shinbo H,Kurita Y,Takada S,Imanishi T,Otsuka A,Furuse H, et al.Resistive index as risk factor for acute urinary retention in patients with benign prostatic hyperplasia.Urology 2010; 76:1440-5.
[9]Galosi AB,Mazzaferro D,Lacetera V,Muzzonigro G,Martino P, Tucci G.Modifications of the bladder wall(organ damage)in patients with bladder outlet obstruction:ultrasound parameters.Arch Italurol 2012;84:263-7.
[10]Cho KS,Kim J,Choi YD,Kim JH,Hong SJ.The overlooked cause of benign prostatic hyperplasia:prostatic urethral angulation.Med Hypotheses 2008;70:532-5.
[11]Cho KS,Kim JH,Kim DJ,Choi YD,Kim JH,Hong SJ.Relationship between prostatic urethral angle and urinary flow rate: its implication in benign prostatic hyperplasia pathogenesis. Urology 2008;71:858-62.
[12]McNeal JE.The prostate and prostatic urethra:a morphologic synthesis.J Urol 1972;107:1008-16.
[13]Ku JH,Ko DW,Cho JY,Oh SJ.Correlation between prostatic urethral angle and bladder outlet obstruction index in patients with lower urinary tract symptoms.Urology 2010;75: 1467-71.
[14]Kuo HC.Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology 1999;54:90-6.
[15]Keqin Z,Zhishun X,Jing Z,Haixin W,Dongqing Z,Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement.Urology 2007;70: 1096-9.
[16]Chia SJ,Heng CT,Chan SP,Foo KT.Correlation of intravesical prostatic protrusion with bladder outlet obstruction.BJU Int 2003;91:371-4.
Received 6 May 2015;received in revised form 21 July 2015;accepted 12 August 2015
Available online 3 September 2015
*Corresponding author.
E-mail address:guwa1986@gmail.com(R.Thekumpadam Puthenveetil).
Peer review under responsibility of Shanghai Medical Association and SMMU.
http://dx.doi.org/10.1016/j.ajur.2015.08.004
2214-3882/?2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier(Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Uroflowmetry;
Tamsulosin;
Ultrasonography; Prostatic urethral angle
 Asian Journal of Urology2015年4期
Asian Journal of Urology2015年4期
- Asian Journal of Urology的其它文章
- GUIDE FOR AUTHORS
- Ureteral stent technology:Drug-eluting stents and stent coatings
- Stellate scar sign of renal cell carcinoma
- Laparoscopic ureterolysis with simultaneous ureteroscopy and percutaneous nephroscopy for treating complex ureteral obstruction after failed endoscopic intervention:A technical report
- Prostate chronic inflammation type IV and prostate cancer risk in patients undergoing first biopsy set:Results of a large cohort study
- Does the presence of a percutaneous renal access influence fluoroscopy time during percutaneous nephrolithotomy?
