A liver donor with double hepatic artery aneurysm: a saved graft
Cagliari, Italy
A liver donor with double hepatic artery aneurysm: a saved graft
Vincenzo Tondolo, Alberto Manzoni and Fausto Zamboni
Cagliari, Italy
The shortage of organs and the increasing median age of deceased donors for orthotopic liver transplantation stimulate transplant centres to accept grafts that otherwise would have been discarded due to severe vascular abnormalities. We encountered a donor with two arterial aneurysms and a left accessory hepatic artery: an arterial aneurysm of the common hepatic artery and a left accessory hepatic artery arising from a second aneurysm of the left gastric artery (Michels type V). A complex reconstruction was created to transplant the liver. Multiple arterial anastomosis was made and the hepatic inflow of the transplanted liver restored. Although the procedure increased the risk of hepatic artery thrombosis, one more organ supposed to be discarded was saved.
liver transplantation;
anastomosis;
anatomy;
hepatic aneurysm;
arterial reconstruction
Introduction
Theshortageoforganshaspushedtransplantsurgeonstoacceptgraftsfromdeceaseddonorsthatotherwisewouldhavebeendiscardedbecauseofseverevascularabnormalities.Theinnovativetechnicalsolutionsmaketheliverstransplantable.[1,2]Wepresentacaseofcomplexarterialabnormalityofthedonordiscoveredatdonorsurgery.Multiplearterialsutureswere necessarytoobtainaneffectivearterialreperfusion.Thecoldischemiatimeandwarmischemiatimewereshort.
Clinical images
A65-year-oldCaucasianwomanwithalcoholiccirrhosis(Child-PughscoreC11,MELDscore25)wasreferredtolivertransplantation.Pre-operativeCTrevealedaMichelstypeVarterialvariation,[3]i.e.aleftaccessoryhepaticarterywasfromtheleftgastricartery.Thedonorwasa69-year-oldmancertifiedtobebrain-deadduetocerebralhemorrhage.Duringthedonorprocedure,aMichelstypeVvariantwasverifiedwithaleftaccessoryhepaticarteryarisingfromananeurysmoftheleftgastricarteryof2.3×2.3cmandasecondaneurysmofthecommonhepaticarteryof2.7×2.5cm(Fig.A).Noothersignificantalterationswerefoundatthesystematicexaminationofthesplenic,mesentericandiliacarteriesofthedonor.Transplantabilityoftheliverwasevaluated.Anen-bloctechniquewasadoptedfortheharvesting.Atthebench-time,asolutionneverdescribedbeforewasadopted.Wecreatedamaincommonarterialtrunkusingfourvascularsutures:thelefthepaticartery(elongation)toatubularsplenicpatch;thesplenicpatchtothegastricstumpofthespleno-gastriccarrefour;thesplenicsideofthecarrefourtotherighthepaticartery;thespleno-gastriccarrefourtoamesentericpatchinordertoobtainagoodarterialstumpfortheanastomosisintherecipient(Fig.B).Totalback-tablelasted125minutes.ThediametersofthearteriesareshowedintheTable.
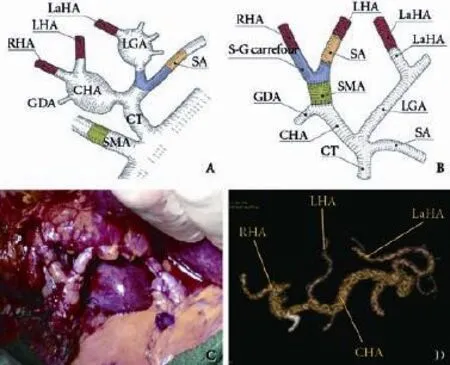
Fig.Arterialreconstruction.A:Anatomyofthedonor;B:Back-tablereconstruction;C:Arterialreperfusion;D:Contrast-enhancedCT3Dreconstructionat36-monthfollow-up.CHA:commonhepaticartery;RHA:righthepaticartery;LHA:lefthepaticartery;LGA:leftgastricartery;GDA:gastroduodenalartery;SMA:superiormesentericartery;LaHA:leftaccessoryhepaticartery;SA:splenicartery;CT:celiactrunk;S-Gcarrefour:spleno-gastriccarrefour.
Astandardpiggy-backtechniquewasusedforthetransplant:cavalanastomosiswascreatedwithpolypropylene3/0,portalsutureinatermino-terminalfashionwithpolypropylene5/0,thenewcommonarterialtrunk(graft)wassuturedtothecommonhepaticarteryatthegastro-duodenaloriginandtheleftaccessoryhepaticarterytothehomologousbranchoftherecipient(Fig.B).Polypropylene7/0runningsuturewasadoptedforallthearterialanastomosisusingoperativemagnificationloops 3.5×(Fig.C).Thecoldischemiatimewas362minutesandwarmischemiatime45minutes.Arterialanastomosisintherecipientlasted15minutesforthemaincommontrunkand18minutesfortheleftaccessoryhepaticartery.BiliarydrainagewasaccomplishedbyaRouxen-Ycholedochojejunostomywithapolydioxanonesuture.Post-operativecoursewasuneventfulwiththepatientonaspirinsince12thdaypost-operationwhenplateletcountexceeded100×109/Lasstandardmanagementinourcenterinaccordancewiththeliterature.[4]Atthetimeofdischarge,liverfunctionwasgoodwithbilirubin2.7mg/dL,AST/ALT42/71IU/L,andINR1.1.After36monthsoffollow-up,thepatientisingoodconditionswithnormalbiochemistry.Contrast-enhancedCT3Dreconstruction(MDCT-64;GEHEALTHCAREbeforeandaftercontrastinfusionwithMIP3Dreconstruction)showedarterialpatencywithoutanystrictureand/orkinkingofthereconstructedarteries(Fig.D).
Discussion
Theincreasingmedianageofdeceaseddonorsandtheincreasingfrequencyofmanagevascularsevereabnormalitiesnowadaysstimulatetransplantcenterstobereadytomanagesuchvascularvariationsandproblemswithsuccess.[3,5]Inthepresentcase,thetimeofthearterialreconstructionwasevaluatedcarefullyinrelationtotheneedtocreateasinglearterialtrunkfromthelefthepaticarteryandrighthepaticarteryandcutdownstreamoftheaneurysm,whichwereveryshortandfarbetweenthemselves.Atback-table,withtheliverintheupsidedownposition,thesutureofsmallarteriesandconduits(Table)asthetubularsplenicpatchorlefthepaticarteryandrighthepaticarterywaseasier,fasterandprecisewithanexcellentresult.Wecouldreperfusetheliverafterportalanastomosisandperformarterialreconstructionlater.Thiswouldhavereducedtheoreticallycoldischemiatime,butgiventhecomplexreconstructionplannedandnecessarytosavearterialinflowofthegraft,thesequencewasassessedasunsafe.Inouropinion,itwasrelatedtothefixedpositionofthegraftintherecipientandtheconsequentseverediscomfortoftheoperatortoperformsuchmultiplesutures,significantlyincreasingvascularrisk.Moreover,wetookintoaccountthatperformingportalreperfusionbeforethearterialreconstructioninthiscasecouldincreaseverymuchtheriskofwarmischemicdamageofbileducts,wherebloodsupplydependssolelyonthehepaticartery.Wecouldhavechosentoligatetheleftaccessoryhepaticarterywithoutantastomosiswithitbut,giventhelargevolumeofthelefthepaticlobeandthelargecalibreoftheleftaccessoryhepaticarteryinrelationtothelefthepaticartery(Fig.C),weestimatedthattheriskofischemiaoftheleftliverwastoohigh,especiallyreferringtotheleftbileductsystem.
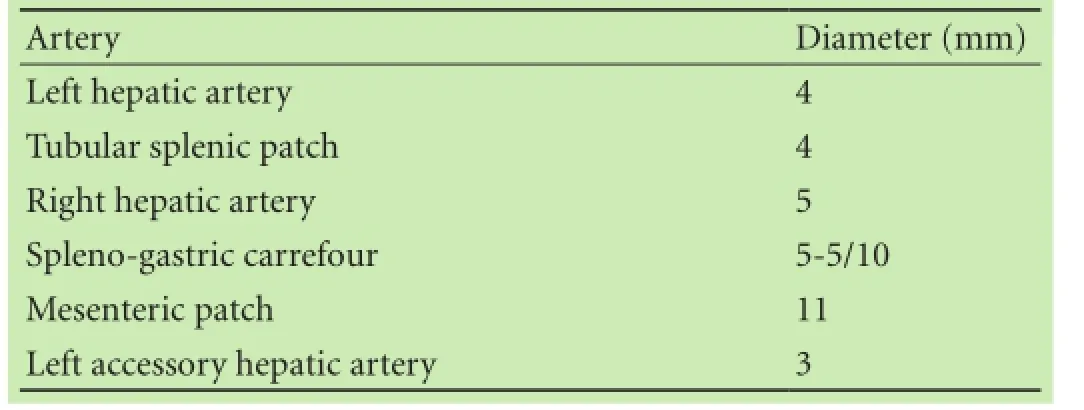
Table.Diametersofarteries
Thesuccessofthiscaseimpliedthatincaseofseverearterialanatomicalalterationoftheliverthatrequiresmultiplearterialanastomosistorestorehepaticinflow,thegraftcanbeused,givinganincreasedbutacceptableriskofhepaticarterythrombosis.
Acknowledgement:TheauthorsthankMarioCostantiniforhishelpinthepreparationoffigures.
Contributors:TVproposedthestudyandwrotethefirstdraft.MAcollectedandanalyzedthedataofthestudy.Allauthorscontributedtothedesignandinterpretationofthestudyandtofurtherdrafts.ZFsupervisedthestudyandfurtherdrafts.TVistheguarantor.
Funding:None.
Ethical approval:Notneeded.
Competing interest:Nobenefitsinanyformhavebeenreceivedorwillbereceivedfromacommercialpartyrelateddirectlyorindirectlytothisarticle.
1BekkerJ,PloemS,deJongKP.Earlyhepaticarterythrombosisafterlivertransplantation:asystematicreviewoftheincidence,outcomeandriskfactors.AmJTransplant2009;9:746-757.
2diFrancescoF,PaganoD,EcheverriG,DeMartinoM,SpadaM,GridelliBG,etal.Selectiveuseofextendedcriteriadeceasedliverdonorswithanatomicvariations.AnnTransplant 2012;17:140-143.
3MichelsNA.Neweranatomyoftheliveranditsvariantbloodsupplyandcollateralcirculation.AmJSurg1966;112:337-347.
4ShayR,TaberD,PilchN,MeadowsH,TischerS,McGillicuddyJ,etal.Earlyaspirintherapymayreducehepaticarterythrombosisinlivertransplantation.TransplantProc2013;45:330-334.
5MartinsPN.Livergraftvascularvariantwith3extra-hepaticarteries.HepatobiliaryPancreatDisInt2010;9:319-320.
Received April 5, 2014
Accepted after revision July 14, 2014
Ifamanemptieshispurseintohishead,nomancantakeitawayfromhim,aninvestmentinknowledgealwayspaysthebestinterest.
—Benjamin Franklin
(Hepatobiliary Pancreat Dis Int 2015;14:443-445)
AuthorAffiliations:DivisionofGeneralSurgeryandTransplantation,DepartmentofSurgery,BrotzuHospital,p.leRicchi,1-09100,Cagliari,Italy(TondoloV,ManzoniAandZamboniF)
VincenzoTondolo,MD,DivisionediChirurgiaGeneraleeTrapiantiOspedaleBrotzu,p.leRicchi,1-09100,Cagliari,Italy(Tel:+39-070-539611;Fax:+39-070-539646;Email:etondolo@hotmail.com)
?2015,HepatobiliaryPancreatDisInt.Allrightsreserved.
10.1016/S1499-3872(14)60325-8
PublishedonlineOctober27,2014.
 Hepatobiliary & Pancreatic Diseases International2015年4期
Hepatobiliary & Pancreatic Diseases International2015年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- Impact of venous thromboembolism on the natural history of pancreatic adenocarcinoma
- Pancreaticoduodenectomy with portal vein/superior mesenteric vein resection for patients with pancreatic cancer with venous invasion
- Influence of comorbidity on outcomes of older patients with acute pancreatitis based on a national administrative database
- A serum metabolomic analysis for diagnosis and biomarker discovery of primary biliary cirrhosis and autoimmune hepatitis
- The response of Golgi protein 73 to transcatheter arterial chemoembolization in patients with hepatocellular carcinoma may relate to the influence of certain chemotherapeutics
