Rapid progression of nonculprit coronary lesions six weeks after successful primary PCI in culprit artery:a case report
Jinjin Tng,Zemu Wng,Dingguo Zhng,Linsheng Wng,?
aDepartment of Cardiology,The First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China;
bDivision of Cardiology,The Affiliated Jiangyin Hospital of Southeast University Medical College,Wuxi,Jiangsu 214400,China.
Rapid progression of nonculprit coronary lesions six weeks after successful primary PCI in culprit artery:a case report
Jianjin Tanga,b,△,Zemu Wanga,△,Dingguo Zhanga,Liansheng Wanga,?
aDepartment of Cardiology,The First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China;
bDivision of Cardiology,The Affiliated Jiangyin Hospital of Southeast University Medical College,Wuxi,Jiangsu 214400,China.
We report a case of a 49-year-old man who was admitted with a 3-hour history of sudden onset of substernal chest pain.Coronary angiography revealed that the left circumflex artery(LCX)was acutely and totally occluded at the mid-portion.In addition,the proximal and mid-portion of the right coronary artery(RCA)had a 60%occlusion.We inferred that the LCX was the culprit artery and primary PCI was successfully performed.Six weeks later, the patient had an eventful course with recurrence of chest pain.Coronary angiography showed no significant stenosis in the previous LCX lesion,while the proximal and middle potion of the RCA had a 90%occlusion.Our case demonstrates the systemic nature of acute coronary syndromes and highlights the inherent instability of coronary artery disease.
acute coronary syndrome,percutaneous coronary intervention,nonculprit coronary lesions
INTRODUCTION
Plaque rupture or endothelial erosion with subsequent occlusive thrombus formation is the primary cause of acute coronary syndrome(ACS)[1-2].It has been generally accepted that plaque vulnerability is an underlying mechanism for this local phenomenon. However,plaque instability may reflect a pan-vascular process with the potential to destabilize the plaques in nonculprit areas[3].Several studies have suggested that vulnerable plaques exist at nonculprit lesions,as well as in the culprit site in ACS patients[4].Moreover, ACS patients who underwent percutaneous coronary intervention(PCI)had a similar recurrent adverse cardiac event rate in culprit lesions and nonculprit lesions (12.9%versus 11.6%during a 3-year follow-up period)[5].Therefore,detection of these non-obstructive, vulnerable plaques may play an important role in the prevention of acute myocardial infarction(AMI)and sudden cardiac death.
CASE REPORT
A 49-year-old man was admitted with a 3-hour history of sudden onset of substernal chest pain.The pain started while he was doing exercise.It was sharp,substernal and associated with shortness of breath and diaphoresis.He had an irregular medical history of hypertension for 5 years and hypertriglyceridemia for 12 years,and had a long history of smoking and drinking.He had no history of spontaneous bleeding,diabetes mellitus,stroke,atrial fibrillation,or familyhistory of coronary artery disease.On admission,his cardiac enzymes,including myoglobin,were normal. His initial electrocardiogram(ECG)showed ST-segment elevation in the inferior(II,III,and avF)and posterior(V7-V9)leads(Fig.1),while there was ST-segment depression in the anterior(V1-V4)leads, which may indicate acute inferior and posterior myocardial infarction.The patient underwent primary angioplasty after receiving aspirin(300 mg)and clopidogrel(300 mg).Coronary angiography revealed that the left circumflex artery(LCX)was acutely and totally occluded at the mid-portion(Fig.2A)and the proximal and mid-portion of the right coronary artery (RCA)had a 60%occlusion(Fig.2B).We inferred that the LCX was the culprit artery and intervention was performed.After percutaneous transluminal coronary angioplasty(PTCA)was carried out in the LCX,lesions of the LCX had a hazy filling defect, which suggested an acute thrombus,and thrombus aspiration was conducted.Then,the patient had a successful stent in the culprit LCX.The patient′s symptoms and postoperative ECG results were significantly improved.One day later,laboratory tests showed: total cholesterol(TC)3.83 mmol/L,triglycerides(TG) 5.35 mmol/L,high density lipoprotein(HDL) 0.75 mmol/L,low-density lipoprotein cholesterol (LDL)2.25 mmol/L,lipoprotein a(Lp(a))179 mg/L, uric acid(UA)445 μmol/L,and NT-proBNP 759 ng/L. A 2D-echocardiogram was performed and showed left ventricular ejection fraction(LVEF)of 67.8%,with no regional wall motion or valvular abnormalities.He remained stable throughout his hospital stay and recovered without any symptoms.The patient was discharged home 12 days later on aspirin(100 mg qd),clopidogrel (75 mg qd),atorvastatin(20 mg qn),ezetimibe(10 mg qd),and trimetazidine(20 mg tid).
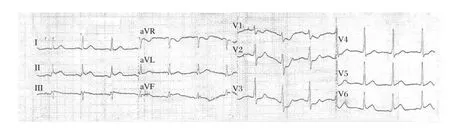
Fig.1Initial electrocardiogram of a 49-year-old man with a 3-hour history of sudden onset of substernal chest pain.
Three weeks post discharge,he recovered without any symptoms and the test results showed values of: TC 2.89 mmol/L,TG 3.31 mmol/L,HDL 0.82 mmol/ L,LDL 1.76 mmol/L,Lp(a)45 mg/L,and UA 460.3 μmol/L.However,one week later,the patient had an eventful course with recurrence of chest pain. ECG showed that R waves of II,III,and avF leads were flat,and exhibited QS model of V7-V9 leads.His cardiac enzymes were still normal.2D-Echocardiography examination showed that left ventricular lateral wall motion had decreased and LVEF was 57.1%.ECT showed myocardial ischemia and regional wall motion abnormalities in the left ventricular lateral wall,as well as inferior wall.Coronary angiography showed no significant stenosis in the previous LCX lesion,while the proximal and middle potion of the RCA had a 90% occlusion(Fig.2C).Two coronary stents were implanted in the RCA.After the procedure,the patienthad a stable course with no recurrence of chest pain.He was discharged six days later.
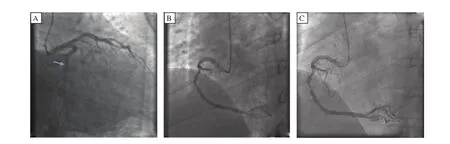
Fig.2Coronary angiography.A:The left circumflex artery was acutely and totally occluded at the mid-portion.B:The proximal and mid-portion of the right coronary artery had a 60%occlusion.C:The proximal and mid-portion of the right coronary artery had a 90%occlusion.
DISCUSSION
It is known that ACS patients are at high risk for recurrent ischemic events caused by a lesion that is anatomically unrelated to the initial event[6].Our case supports the concept that ACS is a pan-vascular process with a higher prevalence of vulnerable plaques in nonculprit sites,leading to recurrent ischemic events in the future.Most(83.3%)of the plaque ruptures of nonculprit artery in a previous study were observed in ST-elevation MI patients[7].Rioufol et al.reported plaque ruptures somewhere other than the culprit lesion in 79%of patients with ACS[8].PCI patients with nonculprit coronary lesions underwent additional clinically driven PCI at rates of 7.7%at 1 year,14%at 2 years, and 16%at 3 years because of the progression of preexisting nonculprit coronary lesions[9].
Because of the rarity of the condition,no management guidelines exist.Nonculprit artery in AMI slows flow globally,which is associated with adverse outcomes[10].Fractional flow reserve assessed by intracoronary pressure wire is useful in deciding whether to revascularize angiographically moderate nonculprit lesions in patients with ACS[11-12].Previous studies have shown that inflammation plays a pivotal role in the development of atherosclerosis and inflammation factors such as C-reactive protein are involved in the progression of nonculprit lesions[13-14].ACS correlates with systemic markers of inflammation,so high recurrent events may be related to additional vulnerable lesions distant from the culprit lesion.These observations support the concept that plaque instability is not merely a local vascular accident but rather probably reflects more generalized pathophysiological processes with the potential to destabilize atherosclerotic plaques throughout the coronary tree.
Despite achieving very low levels of LDL-C,many patients continue to show disease progression[15].Poor lipid profiles at baseline PCI confer significant risks for clinically driven PCI[16].On-treatment TG<150 mg/dl was independently associated with a lower risk of recurrent coronary heart disease(CHD)events,lending support to the concept that achieving low TG may be an additional consideration beyond low LDL-C in patients after ACS[17].Hyperinsulinemia is associated with an increased lipid content and a greater plaque volume of nonculprit intermediate lesions in nondiabetic patients with ACS,suggesting that plaque vulnerability is increased in this subgroup of patients[18].ACS,multivessel diseases,HDL-C and smaller increases in HDL-C were associated with the progression of nonculprit coronary lesion[3,6,17].This finding highlights the need for intensivemodificationofglobalriskinpatientswithcoronary artery disease.
Thrombus was identified more frequently in infarctrelated arteries than non-infarct-related artery lesions in the previous study[7].However,5.0%of the nonculprit coronaries also exhibited thrombus[3,19].These reports all primarily showed that lesion-specific morphologies determined plaque instability and patient symptoms.
Pathological studies have reported that healed ruptured plaque is associated with lesion progression. Subclinical episodes of plaque disruption,local thrombin activation,and subsequent healing with incorporation of thrombus into the vessel wall may represent one pathway for episodic progression superimposed on the slower systemic process[20].This concept is supported by previous angiographic studies showing rapid progression of stenosis with complex angiographic features.After successful PCI of all angiographically significant lesions,overall untreated atherosclerotic burden remains high,and plaque burden lesions are frequently present in the proximal and mid-coronary tree.Patients with plaque burden lesions have greater atherosclerosis throughout the coronary tree,have more thin-cap fibroatheromas,and are at increased risk for future cardiovascular events[21].
To sum up,plaque disruption and healing occur not only at the culprit lesion but may be a pan-coronary process in patients with AMI.We identified some questions regarding the nonculprit coronary.The first concerns vulnerable plaques identified by the imaging tools.Three such devices have emerged and received the USA Food and Drug Administration approval with‘‘tool’’claims that are theoretically capable of identifying certain characteristics of a thin cap fibroatheroma: radiofrequency intravascular ultra-sound(RF-IVUS), optical coherence tomography(OCT),and near-infrared spectroscopy(NIRS).However,each has its advantages and disadvantages[22].So,how should these imaging tools be validated as potential detectors of vulnerable plaque?Secondly,most patients with coronary atherosclerosis are already prescribed high-dose statins. Despite attainment of an LDL-C level of less than 1.8 mmol/L,nonculprit coronary lesions had still progressed,mainly in preexisting nonculprit artery lesions rather than de novo nonculprit artery lesions.One previous study demonstrated that early aggressive lipidlowering therapy,via atorvastatin for 6 months,significantly reduced the plaque volume in patients with ACS[23].We recommend intensive treatment for the culprit lesion and other severe lesions after careful consideration,in a staged fashion if necessary.Thirdly,multivessel PCI for patients during AMI is currently controversial.Onemeta-analysissupportscurrentguidelines discouraging performance of multivessel primary PCI for STEMI.When significant nonculprit vessel lesions are suitable for PCI,they should only be treated during staged procedures[24].One study suggests that multivessel PCI is effective and safe for Chinese patients with ST-segment elevation AMI and simple lesions in nonculprit arteries[25].However,other research showed that initial multivessel PCI was associated with significantlyincreasedriskofin-hospitaldeath,all-causedeath, and MACCE[26].
In conclusion,randomized trials must ultimately be undertaken in patients with high-risk plaques to evaluate the use of either new more potent systemic therapies or focal/regional interventional therapies to demonstrate that treating vulnerable plaques before rupture is effective in preempting future ACS.Here,we describe the clinical presentation and interesting angiographic findings in a case of rapid progression of RCA lesions six weeks after successful primary PCI in the totally occlusion of the mid-portion of the LCX with a brief discussion of a possible mechanism in the context of current management options.This case report demonstrates the systemic nature of acute coronary syndromes,highlights the inherent instability of coronary artery disease,and supports the notion of aggressive secondary prevention in these patients.
[1] Davies MJ,Thomas AC.Plaque fissuring:the cause of acute myocardial infarction,sudden ischaemic death,and crescendo angina.Br Heart J 1985;53:363-73.
[2] Kusama I,Hibi K,Kosuge M,Nozawa N,Ozaki H,Yano H,et al.Impact of plaque rupture on infarct size in ST-segment elevation anterior acute myocardial infarction.J Am Coll Cardiol 2007;50:1230-7.
[3] Asakura M,Ueda Y,Yamaguchi O,Adachi T,Hirayama A,Hori M,et al.Extensive development of vulnerable plaques as a pan-coronary process in patients with myocardial infarction:An angioscopic study.J Am Coll Cardiol 2001;37:1284-8.
[4] Rioufol G,Finet G,Ginon I,Andre-Foue¨t X,Rossi R, Vialle E,et al.Multiple atherosclerotic plaque rupture in acute coronary syndrome:A three-vessel intravascular ultrasound study.Circulation 2002;106:804-8.
[5] Goldstein JA,Demetriou D,Grines CL,Pica M,Shoukfeh M,O′Neill WW.Multiple complex coronary plaques in patients with acute myo-cardial infarction.N Engl J Med 2000;343:915-22.
[6] Stone GW,Maehara A,Lansky AJ,de Bruyne B,Cristea E,Mintz GS,Mehran R,et al.A prospective natural-history study of coronary atherosclerosis.N Engl J Med 2011;364:226-35.
[7] Kotani J,Mintz GS,Castagna MT,Pinnow E,Berzingi CO,Bui AB,et al.Intravascular ultrasound analysis of infarct-related and non-infarct-related arteries in patients who presented with an acute myocardial infarction. Circulation 2003;107:2889-93.
[8] Rioufol G,Finet G,Ginon I,Andre-Foue¨t X,Rossi R, Vialle E,et al.Multiple atherosclerotic plaque rupture in acute coronary syndrome:a three-vessel intravascular ultrasound study.Circulation 2002;106:804-8.
[9] Park MW,Seung KB,Kim PJ,Park HJ,Yoon SG,Baek JY,et al.Long-term percutaneous coronary intervention rates and associated independent predictors for progression of nonintervened nonculprit coronary lesions.Am J Cardiol 2009;104:648-52.
[10]Gibson CM,Ryan KA,Murphy SA,Mesley R,Marble SJ,Giugliano RP,et al.Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction.The TIMI Study Group.Thrombolysis in myocardial infarction.J Am Coll Cardiol 1999;34:974-82.
[11]Ntalianis A,Sels JW,Davidavicius G,Tanaka N,Muller O,Trana C,et al.Fractional flow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial infarction.JACC Cardiovasc Interv 2010;3:1274-81.
[12]Lopez-Palop R,Carrillo P,Torres F,Lozano I,Frutos A, Avanzas P,et al.Results of fractional flow reserve measurement to evaluate nonculprit coronary artery stenoses in patients with acute coronary syndrome.Rev Esp Cardiol(Engl Ed)2012;65:164-70.
[13]Nakachi T,Kosuge M,Hibi K,Ebina T,Hashiba K, Mitsuhashi T,et al.C-reactive protein elevation and rapid angiographic progression of nonculprit lesion in patients with non-ST-segment elevation acute coronary syndrome. Circ J 2008;72:1953-9.
[14]Otake H,Shite J,Shinke T,Watanabe S,Tanino Y, Ogasawara D,et al.Relation between plasma adiponectin, high-sensitivity C-reactive protein,and coronary plaque components in patients with acute coronary syndrome. Am J Cardiol 2008;101:1-7.
[15]Yin ZX,Zhou YJ,Liu XL,Han HY,Yang SW.Clinical predictors for progression of nonintervened nonculprit coronary lesions despite low-density lipoprotein cholesterol less than 1.8 mmol/l after successful stent implantation.Coron Artery Dis 2011;22:49-54.
[16]Park MW,Seung KB,Kim PJ,Park HJ,Yoon SG,Baek JY,et al.Long-term percutaneous coronary intervention rates and associated independent predictors for progression of nonintervened nonculprit coronary lesions.Am J Cardiol 2009;104:648-52.
[17]Miller M,Cannon CP,Murphy SA,Qin J,Ray KK, Braunwald E;PROVE IT-TIMI 22 Investigators.Impact of triglyceride levels beyond low-density lipoprotein cholesterol after acute coronary syndrome in thePROVE IT-TIMI 22 trial.J Am Coll Cardiol 2008;51:724-30.
[18]Mitsuhashi T,Hibi K,Kosuge M,Morita S,Komura N, Kusama I,et al.Relation between hyperinsulinemia and nonculprit plaque characteristics in nondiabetic patients with acute coronary syndromes.JACC Cardiovasc Imaging 2011;4:392-401.
[19]Kotani J,Mintz GS,Castagna MT,Pinnow E,Berzingi CO,Bui AB,et al.Intravascular ultrasound analysis of infarct-related and non-infarct-related arteries in patientswho presented with an acute myocardial infarction. Circulation 2003;107:2889-93.
[20]Ojio S,Takatsu H,Tanaka T,Ueno K,Yokoya K, Matsubara T,et al.Considerable time from the onset of plaque rupture and/or thrombi until the onset of acute myocardial infarction in humans:coronary angiographic findings within 1 week before the onset of infarction. Circulation 2000;102:2063-9.
[21]McPherson JA,Maehara A,Weisz G,Mintz GS,Cristea E,Mehran R,et al.Residual plaque burden in patients with acute coronary syndromes after successful percutaneous coronary intervention.JACC Cardiovasc Imaging 2012;5(S3):76-85.
[22]Stone GW.In search of vulnerable plaque.Circ Cardiovasc Imaging 2012;5:428-30.
[23]Okazaki S,Yokoyama T,Miyauchi K,Shimada K,Kurata T,Sato H,et al.Early statin treatment in patients with acute coronary syndrome:demonstration of the beneficial effect on atherosclerotic lesions by serial volumetric intravascular ultrasound analysis during half a year after coronary event: the ESTABLISH Study.Circulation 2004;110:1061-8.
[24]Jeger RV,Pfisterer ME.Primary PCI in STEMI-dilemmas and controversies:multivessel disease in STEMI patients.Complete versus Culprit Vessel revascularization in acute ST-elevation myocardial infarction.Minerva Cardioangiol 2011;59:225-33.
[25]Xu F,Chen YG,Li JF,Li GS,Ji QS,Lv RJ,et al. Multivessel percutaneous coronary intervention in Chinese patients with acute myocardial infarction and simple nonculprit arteries.Am J Med Sci 2007;333:376-80.
[26]Abe D,Sato A,Hoshi T,Takeyasu N,Misaki M,Hayashi M,et al.Initial culprit-only versus initial multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction:results from the Ibaraki Cardiovascular Assessment Study registry.Heart Vessels 2013[Epub ahead of print].
Received 07 October 2013,Revised 03 November 2013,Accepted 03 December 2013,Epub 15 March 2014
This work was supported by a grant from the National Natural Science Foundation of China(No.81270255).
△Jian-Jin Tang and Ze-Mu Wang contributed equally to this work.
?Corresponding author:Liansheng Wang,MD,PhD,Department ofCardiology,The First Affiliated Hospital of Nanjing Medical University, 300 Guangzhou Road,Nanjing,Jiangsu 210029,China.Tel:+86 25 83724440,E-mail:drlswang@njmu.edu.cn.
The authors reported no conflicts of interests.
?2014 by the Journal of Biomedical Research.All rights reserved.
10.7555/JBR.28.20130155
 THE JOURNAL OF BIOMEDICAL RESEARCH2014年2期
THE JOURNAL OF BIOMEDICAL RESEARCH2014年2期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Naringin ameliorates acetic acid induced colitis through modulation of endogenous oxido-nitrosative balance and DNA damage in rats
- IRE1α is essential for Xenopus pancreas development
- Application of the back-error propagation artificial neural network (BPANN) on genetic variants in the PPAR-γ and RXR-α gene and risk of metabolic syndrome in a Chinese Han population
- Clopidogrel improves aspirin response after off-pump coronary artery bypass surgery
- Diagnostic and prognostic value of minor elevated cardiac troponin levels for percutaneous coronary intervention-related myocardial injury:a prospective,single-center and double-blind study
- A clinical perspective on mucoadhesive buccal drug delivery systems
