Adult Klebsiella pneumoniae meningitis in Qatar: clinical pattern of ten cases
Fahmi Yousef Khan, Mohammed Abukhattab, Mohammed AbuKamar, Deshmukh Anand
1Department of Medicine, Hamad General Hospital, Doha, Qatar
2Infectious Diseases Division, Department of Medicine, Hamad General Hospital, Doha, Qatar
3Microbiology Laboratory, Hamad General Hospital, Doha, Qatar
Adult Klebsiella pneumoniae meningitis in Qatar: clinical pattern of ten cases
Fahmi Yousef Khan1*, Mohammed Abukhattab2, Mohammed AbuKamar2, Deshmukh Anand3
1Department of Medicine, Hamad General Hospital, Doha, Qatar
2Infectious Diseases Division, Department of Medicine, Hamad General Hospital, Doha, Qatar
3Microbiology Laboratory, Hamad General Hospital, Doha, Qatar
PEER REVIEW
Peer reviewer
Raymond Lin Tzer Pin, Head and Senior Consultant, Microbiology, Department of Laboratory Medicine, National University Health System, Singapore. 5 Lower Kent Ridge Road, Singapore.
Tel: +65 67724565
E-mail: Raymond_TP_Lin@nuhs.edu. sg
Comments
It is important for this type of paper to have clear and justifiable definitions for infection v.s. colonization, antibiotic resistance and outcome. The authors have carefully done this, so as a case series, the objectives, methods and results have been presented quite well, and the discussion is appropriate. The authors acknowledge that number of patients is small, but it is remarkable that they have even collected 10 cases over a few years. The documentation of the outcome is good for clinical understanding of the condition.
Details on Page 672
Objective:To describe the clinical presentation, underlying diseases, antimicrobial susceptibility, treatment and outcome of Klebsiella pneumoniae meningitis patients.
Nosocomial meningitis, Community-acquired meningitis, Klebsiella pneumoniae meningitis
1. Introduction
Klebsiella pneumoniae(K. pneumoniae) is a Gramnegative, non-motile, encapsulated, lactose-fermenting, facultative anaerobic, bacillus. Although found in the normal flora of the mouth, skin, and intestines, it can cause diverse infections, including pneumonia, genitourinary tract infection, intraabdominal infection, bacteremia and neonatal meningitis. Recently, it has gained an increasingly important role in adult meningitis both in community acquired and nosocomial settings with significant geographical diversity in its clinical patterns in different parts of the world[1]. In Taiwan, Hong Kong and Thailand,K. pneumoniaeis increasingly being recognized as important pathogens of community-acquired meningitis[1-4], while it is uncommon in the USA, Cuba, Europe and othercountries[5-8].K. pneumoniaemeningitis is seen mostly in patients with diabetes mellitus, debilitating diseases, extrameningealK. pneumoniaeinfection,K. pneumoniaebacteremia, and patients with head injury or who have undergone a neurosurgical procedure[1].
In the state of Qatar, there is lack of information aboutK. pneumoniaemeningitis. The aim of this study was to determine the clinical presentation, underlying diseases, antimicrobial susceptibility, treatment and outcome ofK. pneumoniaemeningitis in patients admitted to Hamad general hospital, Qatar.
2. Materials and methods
This retrospective study was conducted at Hamad general hospital, a tertiary hospital with eight operating theatres, six intensive care units and 621 beds. It involved all adult patients with 15 years of age or older who admitted to Hamad General Hospital with culture provenK. pneumoniaemeningitis. To identify the patients, we reviewed the cerebrospinal fluid (CSF) cultures registered in the microbiology laboratory from January 1, 2007 to December 31, 2012. The files of the patients were reviewed retrospectively to retrieve the following data on a standardized data sheet: clinical picture, demographic data, underlying medical conditions, meantime between the surgery and the onset of the infection, susceptibility tests forK. pneumoniae, antibiotic therapy used, duration of therapy and patient outcome.
Diagnosis ofK. pneumoniaemeningitis was made if the following criteria were fulfilled: (1) the patient hadK. pneumoniaecultured from CSF; (2) the patient had at least one of the following with no other apparent cause: fever (38 °C), headache, meningeal signs, cranial nerve signs or irritability; (3) the patient had at least one of the following alterations in CSF: increased white cells, elevated protein and/or decreased glucose. A positive CSF culture or Gram stain with normal levels of glucose, proteins and cell count in the absence of symptoms was considered as contamination/colonization.
Meningitis was considered as nosocomial if the patient had acquired the infection more than 72 h after hospitalization or within one month after discharge from the hospital where the patient received an invasive procedure, especially a neurosurgical one. Otherwise, the patient was considered to have “community-acquired” infection. Mixed-infection was defined as at least two bacterial organisms isolated concomitantly from CSF culture.K. pneumoniaeisolates were considered as multidrug resistant if they exhibited resistance to at least two antibiotics used in empirical therapy (third and fourth-generation cephalosporins, carbapenems or piperacillin/tazobactam). Empirical antimicrobial therapy was deemed as inappropriate if the antibiotics were administered more than 24 h of CSF collection and/or when the dosage, route and duration of treatment were not in accordance with hospital guidelines. Definitive therapy was considered as appropriate if antimicrobials were modified and administered not later than two hours after the CSF culture was obtained. Intravenous aminoglycoside monotherapy was considered inappropriate because of low penetration into CSF. In-hospital mortality included all causes of death during admission and considered as the main outcome measure of this series.
The results of analyses of continuous variables are expressed as mean±SD unless otherwise specified.
3. Results
There were ten episodes ofK. pneumoniaemeningitis occurring in ten patients during the study period (nine males and one female). The mean age was (43.3±12.8) years (range 20-61 years) and eight were non-Qatari patients. Most patients 80% (8/10) had nosocomial meningitis with neurosurgery being the most frequent associated condition. The mean period between neurosurgery and the onset of the infection was (10.3±3.0) d (range 4-15 d). Table 1 shows the demographic and clinical data of the ten patients.
Fever and altered consciousness were the most frequent symptom (Table 1). Cerebrospinal fluid showed pleocytosis in all cases [mean (1 520±2 998)] with a polymorphonuclear predominance. Elevated protein levels [mean (210±76) mg/ dL] and low glucose levels [(27±8) mg/dL] were also noted. Gram stain showed Gram-negative rods in 50% (5/10) cases, while positive CSF culture results were found in all patients, four (Patients 2, 4, 5, 10) of them had mixed infection.
The antimicrobial susceptibilities ofK. pneumoniaevaried. Multidrug resistance was observed in 2/10 cases, while all isolates were sensitive to gentamicin, meropenem and piperacillin/tazobactam (Table 1). One isolate was extended spectrum beta lactamase (ESBL) producer (detected by the phenotypic confirmatory method). All the patients received appropriate empirical and definitive antibiotic treatments. The mean duration of intravenous antimicrobial treatment was (19.3±7.0) d (range 5-28 d). Intrathecal gentamicin was given for two patients. In addition to medical treatment, all patients with external ventricular drains underwent removal and replacement of the device, while in-hospital mortality was 50% (5/10).
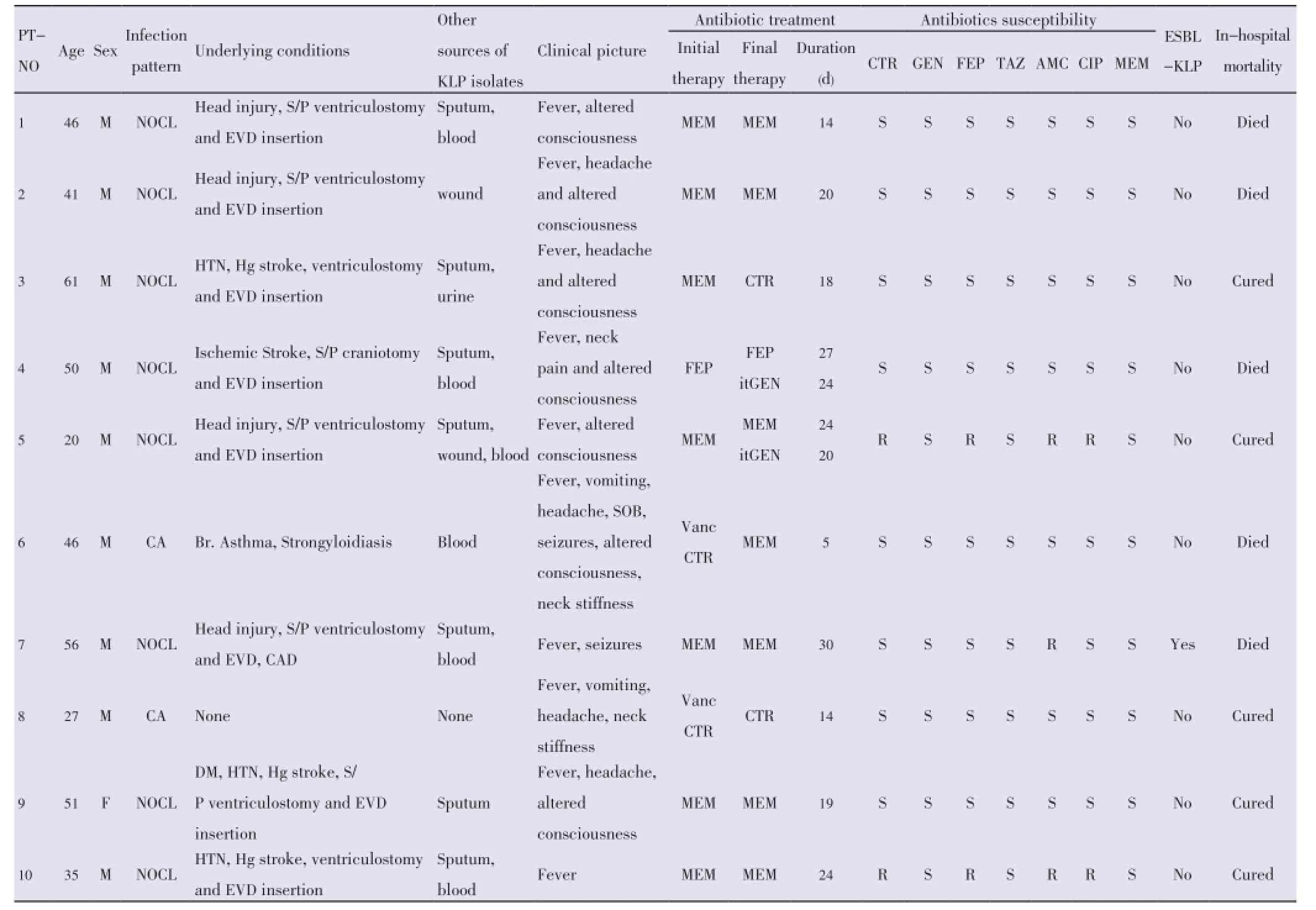
Table 1 Describes the demographic and clinical data of the ten patients.
4. Discussion
In Qatar,K. pneumoniaeis among the most common Gram-negative bacteria encountered by physicians. However, the prevalence ofK. pneumoniaemeningitis is yet unknown.
As noted in this series the majority of the cases were nosocomial, which is comparable with reports from western countries[6,9], but different from those reported in Taiwan[1,2]. All nosocomial cases in this study had a neurosurgical condition as the preceding event and neurosurgical devices as predisposing factors, which may reflect the expansion of neurosurgical services or inadequate infectious control program in our hospital. This finding coincides with many reports worldwide[1-9]. The interval between neurosurgical procedure and the onset of meningitis is (10.3±3.0) d, which is similar to what was mentioned in the literature. On the other hand, a high incidence of DM among patients with adult community-acquired spontaneous bacterial meningitis (38.5%) has been reported in Taiwan[8,9]. In our study, none of the two patients with community-acquired meningitis had diabetes mellitus; we found strongyloidiasis as a predisposing factor in one patient, and no obvious factor could be found in the other. Localized strongyloidiasis, as well as disseminated strongyloidiasis, can predispose individuals to bacterial meningitis with enteric organisms such asK. pneumoniae,Escherichia coliandEnterococcusspp. in the absence of evidence for strongyloidiasis outside the gastrointestinal tract[10].
Similar to other reports[1-9], the clinical picture and CSF (biochemistry and cell count) findings in this series were indistinguishable from other forms of bacterial meningitis. These findings make CSF Gram staining and culturing imperative in all patients. However, the examination of Gram stain on admission can be negative or misleading; because of the small number of organisms, patients being partially treated, and culture time of more than one day may be required, thus delaying the final diagnosis of meningeal infection and representing a prognostic factor of mortality.
Thus, the choice of appropriate empiric therapy whileawaiting results of sensitivity is crucial and should be based on the most common pathogen prevalent in a particular geographical area and age group and their antibiotic susceptibility pattern. According to our local policy, ceftriaxone plus vancomycin are the empirical treatment of choice for community-acquired meningitis, while meropenem is the empirical treatment of choice for nosocomial meningitis. Although the empiric treatment in our study was appropriate in all cases, the mortality was high, which could be resulted from the fact that most of our cases had preceding neurosurgical events. Moreover, we think that post-surgicalK. pneumoniaemeningitis might need intrathecal therapy in addition to the parenteral antibiotics in order to decrease the mortality.
Our study has some limitations. First, it is retrospective/ hospital based. Second, the number of patient is small.
In conclusion, the clinical picture and CSF findings ofK. pneumoniaemeningitis were not different from those of other bacterial meningitis, and the mortality was high. The number of cases in this series was too small to come up with therapeutic and prognostic conclusions. Further largescale prospective study is needed for better description of the management and prognosis of adultK. pneumoniaemeningitis.
Conflict of interest statement
We declare that we have no conflict of interest.
Comments
Background
This is a descriptive paper onKlebsiellameningitis, a rather rare condition, except when occurring in neurosurgical infections. The authors look at the clinical management, progress and outcome of these infections.
Research frontiers
This is a descriptive clinical study and cases have been described before. However, it is an uncommon disease to compilation of a series of clinical cases, which will help build up new knowledge on this subject.
Related reports
Thigpenet al.(2011) has reported the bacterial meningitis in the United States. Anget al. (2011) has study the prognostic factors and outcomes in endogenousK. pneumoniaeendophthalmitis.
Applications
The reported cases can be added to the clinical database on this uncommon condition.
Peer review
It is important for this type of paper to have clear and justifiable definitions for infectionv.s.colonization, antibiotic resistance and outcome. The authors have carefully done this, so as a case series, the objectives, methods and results have been presented quite well, and the discussion is appropriate. The authors acknowledge that number of patients is small, but it is remarkable that they have even collected 10 cases over a few years. The documentation of the outcome is good for clinical understanding of the condition.
[1] Fang CT, Chen YC, Chang SC, Sau WY, Luh KT. Klebsiella pneumoniae meningitis: timing of antimicrobial therapy and prognosis. QJM 2000; 93: 45-53.
[2] Chang WN, Huang CR, Lu CH, Chien CC. Adult Klebsiella pneumoniae meningitis in Taiwan: an overview. Acta Neurol Taiwan 2012; 21: 87-96.
[3] Hui AC, Ng KC, Tong PY, Mok V, Chow KM, Wu A, et al. Bacterial meningitis in Hong Kong: 10-years’ experience. Clin Neurol Neurosurg 2005; 107: 366-370.
[4] Khwannimit B, Chayakul P, Geater A. Acute bacterial meningitis in adults: a 20 year review. Southeast Asian J Trop Med Public Health 2004; 35: 886-892.
[5] Thigpen MC, Whitney CG, Messonnier NE, Zell ER, Lynfield R, Hadler JL, et al. Bacterial meningitis in the United States, 1998-2007. N Engl J Med 2011; 364: 2016-2025.
[6] Logigan C, Mihalache D, Dorneanu O, Turcu T. [Study of nosocomial bacillary meningitis admitted in the clinic of infectious diseases Ia?i on a 20 years period]. Rev Med Chir Soc Med Nat Iasi 2009; 113: 721-726. Romanian.
[7] Pérez AE, Dickinson FO, Rodríguez M. Community acquired bacterial meningitis in Cuba: a follow up of a decade. BMC Infect Dis 2010; 10: 130.
[8] Brouwer MC, Tunkel AR, van de Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin Microbiol Rev 2010; 23: 467-492.
[9] Ang M, Jap A, Chee SP. Prognostic factors and outcomes in endogenous Klebsiella pneumoniae endophthalmitis. Am J Ophthalmol 2011; 151: 338-344.
[10] Sasaki Y, Taniguchi T, Kinjo M, McGill RL, McGill AT, Tsuha S, et al. Meningitis associated with strongyloidiasis in an area endemic for strongyloidiasis and human T-lymphotropic virus-1: a singlecenter experience in Japan between 1990 and 2010. Infection 2013; 41: 1189-1193.
10.12980/APJTB.4.201414B100
*Corresponding author: Dr. Fahmi Yousef Khan, (MD), Consultant, Department of medicine, Hamad General Hospital, Doha, Qatar.
Tel: 0974 4879228; 0974 5275989
Fax: 0974 4392745
E-mail: fakhanqal@yahoo.co.uk
Article history:
Received 3 Jun 2014
Received in revised form 13 Jun, 2nd revised form 20 Jun, 3rd revised form 29 Jun 2014
Accepted 20 Jul 2014
Available online 28 Aug 2014
Methods:This retrospective study involved all patients with 15 years of age or older who admitted to Hamad General Hospital with culture proven Klebsiella pneumoniae meningitis from January 1, 2007 to December 31, 2012.
Results:A total of ten cases were identified (nine males and one female). Their mean age was (43.3±12.8) years. Eight patients (80%) had nosocomial meningitis with neurosurgery being the most frequent associated condition. Fever and altered consciousness were the most frequent symptom. Cerebrospinal fluid showed elevated protein and glucose levels. Gram stain showed Gram-negative rods in 50% of cases, while positive cerebrospinal fluid culture results were found in all patients. Multidrug resistance was observed in two cases, and all patients had received appropriate empirical and definitive antibiotic treatments. The mean duration of intravenous antimicrobial treatment was (19.3±7.0) d and all patients with external ventricular drains underwent removal of the device, while in-hospital mortality was 50%.
Conclusions:The number of cases was too small to come up with therapeutic and prognostic conclusions. Further large-scale prospective study is needed.
 Asian Pacific Journal of Tropical Biomedicine2014年8期
Asian Pacific Journal of Tropical Biomedicine2014年8期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- An overview of travel-associated central nervous system infectious diseases: risk assessment, general considerations and future directions
- Genetic diversity of the msp-1, msp-2, and glurp genes of Plasmodium falciparum isolates along the Thai-Myanmar borders
- Impact of antibacterial drugs on human serum paraoxonase-1 (hPON1) activity: an in vitro study
- High levels of Zinc-α-2-Glycoprotein among Omani AIDS patients on combined antiretroviral therapy
- Toxicity effects of water extracts of Holothuria atra Jaeger in mice
- Prevention of renal dysfunction by nutraceuticals prepared from oil rich plant foods
