Mirizzi Syndrome:Our Experience with 27 Cases in PUMC Hospital
Xie-qun Xu,Tao Hong,Bing-lu Li*,Wei Liu,Xiao-dong He,and Chao-ji Zheng
Department of General Surgery,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
MIRIZZI syndrome (MS) was first described by Pablo L Mirizzi in 1948 which is characterized by common hepatic duct obstruction owing to extrinsic mechanical compression and/or surrounding inflammation by a gallstone impacted at the gallbladder neck or cystic duct.1In some cases,the associated inflammation was found to progress to cholecystocholedochal fistula.The reported prevalence of MS is about 0.06%-3.0%in patients undergoing cholecystectomy.2-4Its clinical manifestations sometimes vary from obstructive jaundice associated with extrinsic compression to cholecystobiliary fistula when the stone migrates through the cystic duct.There are 4 types of MS reported by Csendeset al∶5(Type I) extrinsic compression of the common bile duct by an impacted gallstone at the gallbladder or at the cystic duct;(Type II) cholecystobiliary fistula involving less than one-third of the circumference of the common bile duct;(Type III) cholecystobiliary fistula involving up to two-thirds of the circumference of the common bile duct;(Type IV) cholecystobiliary fistula comprising the whole circumference of the common bile duct.Most of the MS cases are not accurately diagnosed preoperatively,despite of the modern imaging techniques.So there is increased risk of bile duct injury,especially when a fistula,extensive adhesions of the Calot’s triangle,or anatomic alterations makes the surgical intervention more complex.The purpose of this study was to retrospectively review the experience of our center in the diagnosis and treatment of MS over 20 years.
PATIENTS AND METHODS
From January 1988 to November 2011,a total of 8697 cholecystectomies that were performed during the period in Peking Union Medical College (PUMC) Hospital were included in this retrospective review.And 27 patients with the final diagnosis of MS were retrospectively evaluated.The following variables were analyzed∶age,sex,years of gallstone disease,type of MS according to criteria proposed by Csendeset al,5clinical presentations,laboratory findings,diagnostic modalities,presence of choledocholithiasis,type of surgical procedures,intraoperative and postoperative complications and mortality.
RESULTS
General conditions
MS diagnosis was made in 27 patients of the 8697 cholecystectomies with the incidence of 0.31% during the 23 years period.There were 19 (70.4%) female patients and 8 (29.6%)male patients with a mean age of 57.1 (range∶36-79) years.Body mass index was 29.3 (range∶21.1-32.7) kg/m2.The duration of gallstone disease from the onset of symptoms to surgical management was long with a mean period of 10.5(range∶3-19) years.The most frequent signs and symptoms were abdominal pain in 24 (88.9%) patients and jaundice and itching in 21 (77.8%) patients.Other symptoms included nausea and vomiting (44.4%,12/27),fever (37.0%,10/27),anorexia (33.3%,9/27),diarrhea (7.4%,2/27),and constipation (3.7%,1/27).One (3.7%) patient did not have any symptoms at presentation.Table 1 summarizes the laboratory findings at presentation.There were 26 patients with abnormal liver function.
Clinical diagnosis
All 27 patients underwent ultrasonography initially which revealed cholelithiasis and the dilation of the extrahepatic bile duct in all MS patients,and ultrasonography also showed atrophic gallbladder with gallstones in both gallbladder and common bile duct in 13 (48.1%) patients,gallstones only in the gallbladder in the other 14 (51.9%) patients.Dilatedintrahepatic biliary tree was shown in 11 (40.7%) patients.In addition,8 patients were further investigated with computed tomography (CT) of the abdomen to evaluate whether there was a gallbladder cancer.CT showed dilated extrahepatic bile duct in all 8 patients and dilated intrahepatic bile duct in 3 patients.Moreover,9 patients underwent magnetic resonance cholangiopancreatography (MRCP),7 patients’ MRCP showed external compression of hepatic ducts by impacted gallstones and dilatation of the proximal biliary system,and they were suspected with MS.Totally,17 patients underwent endoscopic retrograde cholangiopancreatography(ERCP).The ERCP revealed the stenosis of the extrahepatic bile duct as well as dilation of the intrahepatic biliary tree in all 17 cases,stones within the cystic duct adjacent to bile duct in 17 cases,bile duct stones in 11 cases and pus in bile duct in 3 cases.The sphincterotomy,nasobiliary drain,stent placement,complete and partial stone extraction during the ERCP were performed in 8,9,6,5 and 3 patients,respectively.Preoperatively,there were 12 (12/27,44.4%)cases diagnosed with MS through ultrasonography,4 (4/8,50.0%) cases diagnosed with MS through CT (Fig.1A),7(7/9,77.8%) cases diagnosed with MS through MRCP,and 17 (17/17,100%) cases diagnosed with MS through ERCP(Fig.1B).There were 12 (44.4%) MS Type I cases,9(33.3%) MS Type II cases and 6 (22.2%) MS Type III cases.
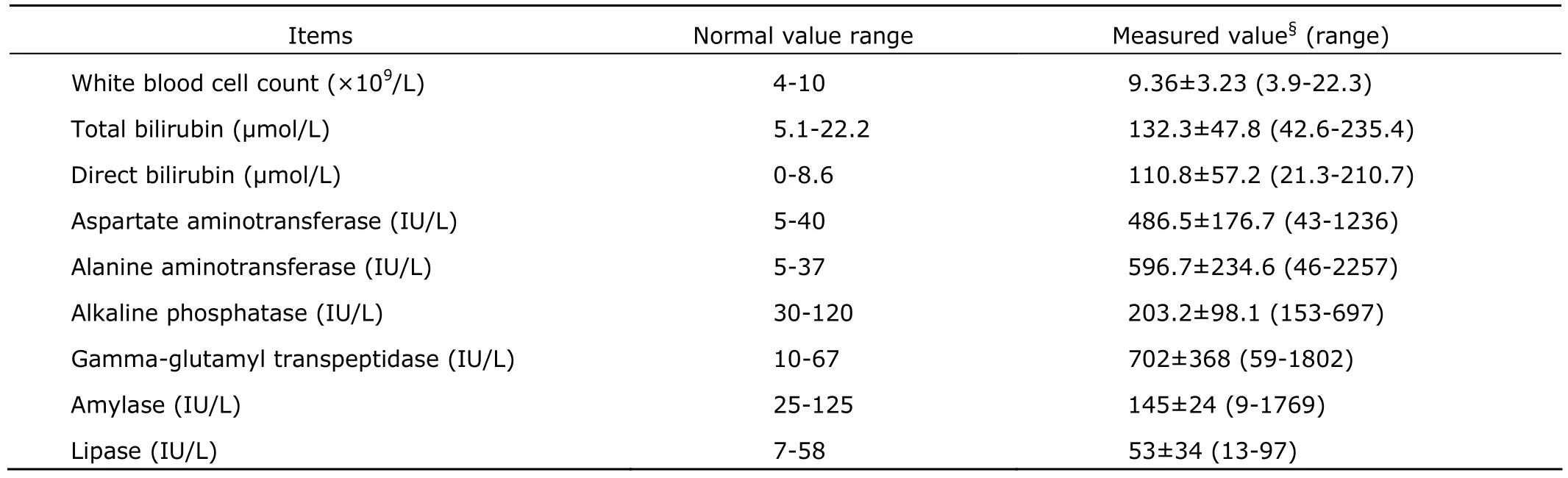
Table 1.Laboratory characteristics at presentation of 27 Mirizzi syndrome patients
Treatment
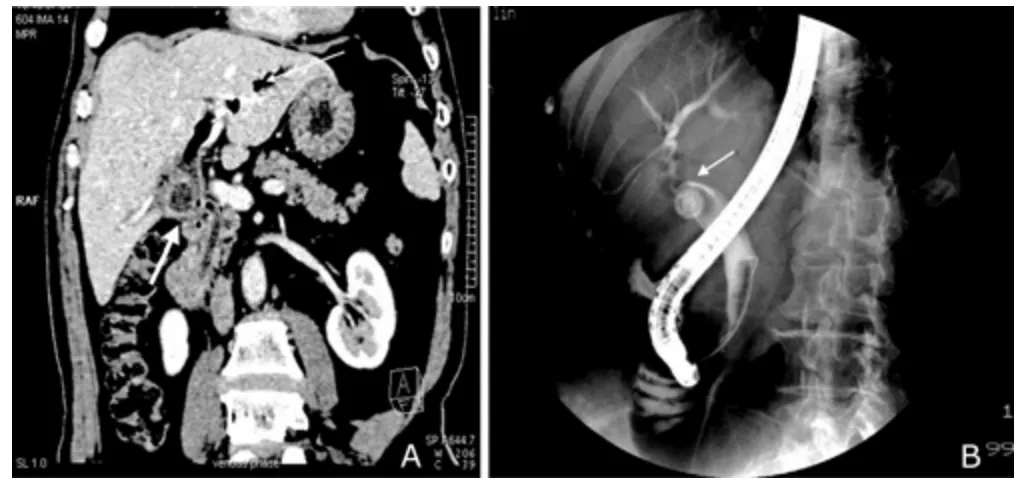
Figure 1.A.Mirizzi syndrome with acute cholangitis.Computed tomography reveals radioparent calculus in the dilated cystic duct (bold arrow),vague structure in the junction of cystic duct,and common hepatic duct with air in the intrahepatic tract (thin arrow).B.Mirizzi syndrome(Type I,Csendes classification).Endoscopic retrograde cholangiopancreatography indicates extrinsic compression of the common hepatic duct (arrow).
Cholecystectomy was performed in all 27 patients.Totally,15 (55.6%) patients started with laparoscopic exploration,but only 3 (11.1%) of the surgeries could successfully be performed with laparoscopic cholecystectomy (LC).The conversion rate from LC to open cholecystectomy (OC) was 80% (12/15).LC was converted to OC technically because of severe adhesion and indistinct anatomy due to peribiliary edematous and inflammatory tissue.Those who underwent successful LC had Type I MS.For those patients who were converted to OC,9 patients had Type I MS and 3 patients had Type II MS,respectively.Of 12 patients with Type I MS,9 simply underwent cholecystectomy including 3 cases receiving LC and 6 undergoing OC.The remaining 3 Type I MS patients (conversion to OC) and 6 Type II MS patients(conversion to OC 3 cases,OC 3 cases) underwent cholecystectomy,T-tube placement with choledochotomy for biliary drainage.The other 3 Type II MS patients receiving LC underwent cholecystectomy,closure of the fistula with gallbladder cuff,T-tube placement.All the 6 patients with Type III MS underwent cholecystectomy with excision of the external bile ducts and Roux-en-Y hepatico-jejunostomy.The operative characteristics of all patients are summarized in Table 2.
Pathological diagnosis
Pathological examinations were done for all surgical specimens.The pathological results were reported as acute or chronic cholecystitis except one patient with incidental gallbladder cancer (stage I),who did not need further treatment.
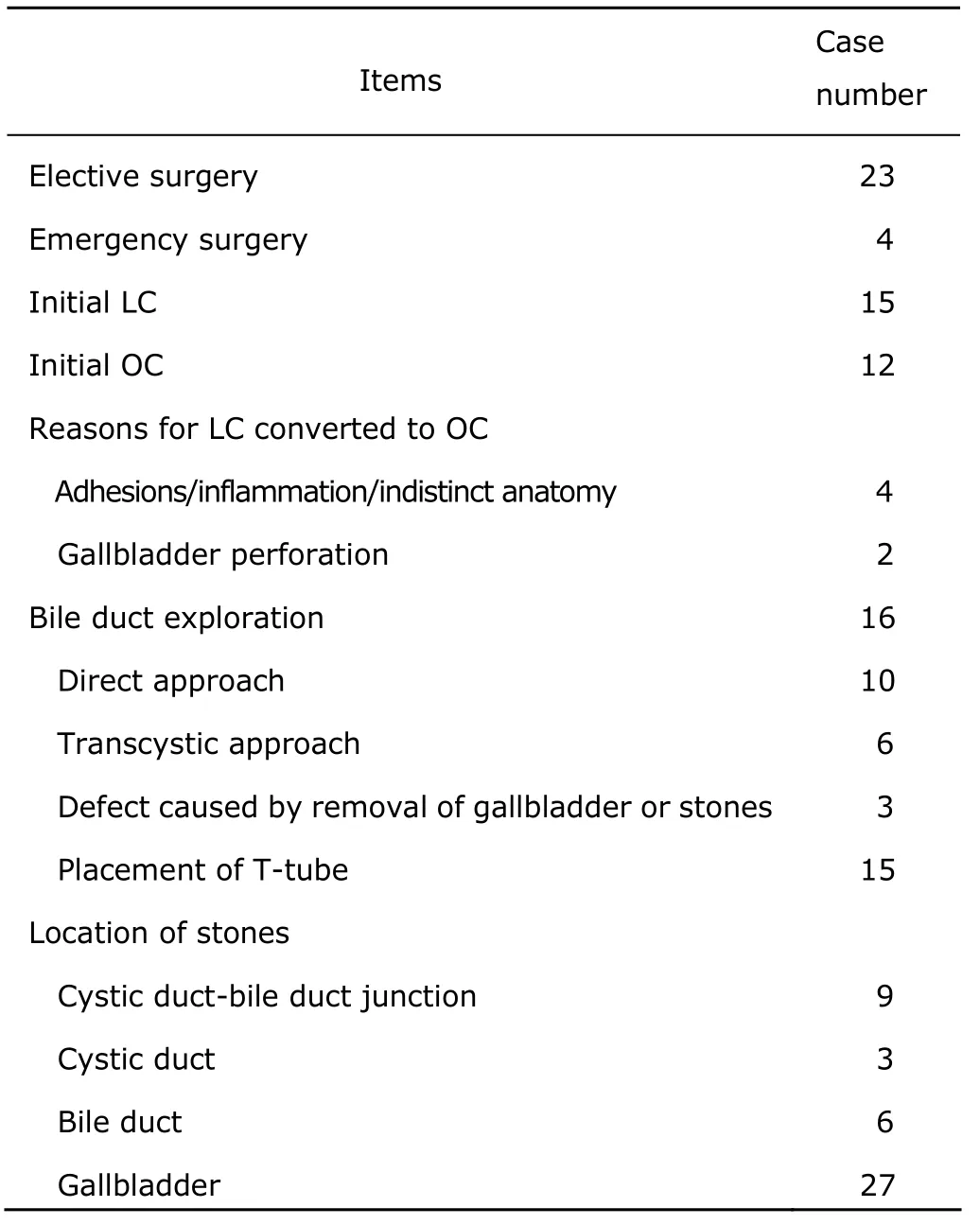
Table 2.Operative characteristics of 27 Mirizzi syndrome patients
Prognosis
The mean hospital stay time was 9.7 (range∶6-21) days.The mean time of follow-up was 35.3 months with a range of 3-146 months.Two patients were lost to follow-up.There was no operative mortality,and no complications in the early postoperative period except 1 case with wound infection.Postoperative T-tube cholangiography was performed in 8 patients,7 patients were normal and 1 showed inflammatory stricture,and it was completely resolved in the repeated T-tube cholangiography with the medical therapy one month later.However,there was 1 (3.7%) patient who underwent the excision of external bile ducts and Roux-en-Y hepatico-jejunostomy had cholangitis which occurred postoperatively 5 month later and recovered with the treatment of antibiotics.All the patients had no late postoperative complications (biliary stricture,infection,etc.) in the follow-up period.
DISCUSSION
The phenomenon as functional hepatic syndrome of MS is a rare cause of acquired jaundice.It is a rare complication of long-standing cholelithiasis associated with large gallstones located in the gallbladder that compresses the common hepatic duct.The obstructive jaundice can be caused by direct extrinsic compression by the stone or from fibrosis caused by chronic cholecystitis inflammation.A cholecystocholedochal fistula may occur.
In 1989,a classification with four types for MS was suggested by Csendeset al5which is widely accepted and on which the surgical management for MS depends.
The incidence of MS is low and the reported prevalence of MS ranges from 0.06% to 3.0%2-4among patients undergoing cholecystectomy.In our study,it was 0.31%which correlates with the incidence rate reported in the literatures.In our study,the most patients with MS was Type I (Type I 44.4%,Type II 33.3%,Type III 22.3%,Type 0),and Chanet al6also reported the same dominance of Type I,whereas Aydinet al7and Csendeset al5reported the dominance of incidence of Type II and Type III,respectively.The difference may be due to more knowledge on MS and early diagnosis with modern diagnostic modalities.The mean age of 27 patients in our study was 57.1 years old (range∶36-79 years),which varies from other reports (range∶44-62 years).5,6But there were 19 (70.4%) female patients which correlates well with other reports.5,6
The clinical diagnosis of MS is difficult due to the absence of reliable clinical indicators.Most cases present with abdominal pain,jaundice,and abnormal liver function tests (more than 75% patients have those abnormalities in our study) which were generally consistent with obstructive choledocholithiasis,but these are neither specific nor diagnostic for the differentiation of MS from other biliary tract disease.
Because of the nonspecific clinical presentations of MS,the preoperative diagnosis of MS with imaging study is also similar.Ultrasonograhpy is used as a noninvasive screening modality which shows the typical features of MS∶shrunken gallbladder with a large gallstone in the gallbladder neck,dilation of the proximal bile duct and intrahepatic bile ducts,and the common bile duct having a normal diameter below the obstruction.Ultrasonography is the most common initially used imaging method in obstructive jaundice with the sensitivity of 8.3%-42%.5,8,9But Wehrmannet al10reported that the intraductal ultrasonography can get a diagnosis with a sensitivity of 97% and a specificity of 100%.
Similar to ultrasonography,CT can not show definite information about MS.CT can often show dilation of intrahepatic and extrahepatic ducts with stones in the biliary trees above the level of gallbladder neck.It can also provide the additional information which is possible to differentiate between MS and malignant lesions of the extrahepatic bile duct and gallbladder.11,12
MRCP is another noninvasive imaging technique which can show the typical features of MS.MRCP can also provide additional information on the adjacent tissue around gallbladder.13
ERCP is the most effective and sensitive imaging modality for the diagnosis of MS.ERCP can clearly depict the anatomical changes that caused by MS,including the curvilinear impression of the impacted gallstone on the common hepatic ducts by extrinsic compression from the gallstone and dilatation of the proximal biliary system.ERCP can also determine whether there is fistula and the location of the biliary obstruction;it can especially provide the biliary therapeutic decompression with papillotomy and stent insertion which serves both diagnostic and therapeutic purposes.9There were 15 patients undergoing preoperatively nasobiliary drain or stent placement (9/6) for cholangitis or deep jaundice in our study.This preoperatively interventional management was reported by Chowbeyet al.14The reflux of bile into the gallbladder is an indicator of the presence of fistula for the cystic duct,which is usually occluded by inflammation.8Cholangiogram in ERCP would help to confirm the presence and the size of the fistula,and stones in the common bile duct could be extracted with sphincterotomy which was performed in 8 patients in this study.
In our study,the sensitivity of ultrasonography,CT,MRCP and ERCP in the preoperative diagnosis of MS was 44.4%,50%,77.8%,and 100%,respectively,which correlates well with previous reports.5,8,9
The surgery is most definite treatment for MS,and must be individualized depending on the type of MS.Since preoperative diagnosis of MS is difficult,both intraoperative recognition and surgical experience remain critical to get a good surgical result without any complications.
For Csendes Type I,different surgical approaches may be feasible because there is no cholecysto-biliary fistula.Most authors agreed that total cholecystectomy can be performed if there is only moderate inflammation when safe dissection is possible.15,16In the case with local inflammation severely hampering safe dissection of the structure of Calot’s triangle,retrograde fundus-first cholecystectomy technique is preferred approach.If safe dissection is not possible,subtotal cholecystectomy with the neck of gallbladder left in pace is another approach.15-17The common bile duct should be explored to exclude further causes of obstruction when there are common bile ducts,fistula or stenosis at the impacted site.The insertion of a T-tube may be needed for temporary biliary decompression.In our study,there were 3 patients with Csendes Type I undergoing cholecystectomy and T-tube placement with choledochotomy in the bile duct successfully.The reported incidence of conversion to OC was very high (37%-78%),7and it was 80% in our study which is very close to the literature.The main reasons for the conversions were due to the severe inflammation and anatomic distortion.
Jaundice is very common in MS Type II-IV for the possible presence of cholecysto-biliary fistula,so they need more complex intervention,but there is less well defined surgical treatment.During the dissection of biliary system,if bile flows out from the common bile duct after the removal of the impacted gallstone in the cystic duct,cholecysto-biliary fistula must be strongly suspected.
The management of MS Type II and III is more controversial.To avoid the lesion of the common bile duct,most of MS Type II can usually be treated with partial cholecystectomy,then with or without oversewing the gallbladder cuff,and closing the fistula with a T-tube placement in the common bile duct.15Some authors also suggested placement of a T-tube through a separate choledochotomy in the distal common bile duct in order to prevent excessive leakage and stricture at the fistula site.18In our study,6 (66.7%) patients with MS Type II received cholecystectomy,T-tube placement with choledochotomy,in which 3 patients underwent closure of the fistula with gallbladder cuff,and the other 3 did not.For repair of large defects (MS Type II and IV),some authors refer a biliary-enteric bypass with a Roux-en-Y hepatico-jejunostomy or a choledochoduodenostomy for large fistula or severely damaged bile duct.4,18,19The 6 patients with MS Type III underwent excision of external bile ducts and Roux-en-Y hepatico-jejunostomy.There was no MS Type IV in our study.
No significant bile leakage was observed postoperatively.One patient (MS Type II) with persistent jaundice underwent ERCP with extraction from the common bile duct after he received cholecystectomy,T-tube placement with choledochotomy one month postoperatively.T-tube would be removed about 8 weeks postoperatively when the cholangiogram through T-tube showed there were no stones or stricture in the common bile duct.All the patients with MS had a mean follow-up time of 35.3 (range∶3-146) months.
In conclusion,the incidence of MS is low.The preoperative diagnosis is critical for surgeons to determine the best surgical procedure.Noninvasive laboratory investigations and ultrasonography,or CT,only provide supportive diagnostic information.A preoperative ERCP or MRCP is usually used to establish the diagnosis and assess the anatomy;especially ERCP can also decompress the obstructive bile duct system.Since the introduction of LC,it is very risky in the treatment of MS with LC.Only experienced surgeons can perform LC on selected MS Type I patients.The open approach remains the standard method for MS Type II-IV due to the complicated situation of extensive adhesions of the Calot’s triangle,or anatomic alterations and the frequent need for biliary enteric drainage.For MS Type I,the surgical treatment generally involves minimal interventions such as partial or total(open or laparoscopic) cholecystectomy.Most of MS Type II and some of the MS Type III defects can usually be treated successfully with either complete or partial cholecystectomy followed by repair of the bile duct defect with gallbladder cuff or choledochoplasty with T-tube placement in the common bile duct.The remaining MS Type II and III cases could undergo cholecystectomy with excision of the external bile ducts and reconstruction with Roux-en-Y hepatico-jejunostomy.For MS Type IV,cholecystectomy with excision of the external bile ducts and reconstruction with Roux-en-Y hepatico-jejunostomy is recommended.
1.Mirizzi PL.Syndrome del conducto hepatico.J Int Chir 1948;8∶731-47.
2.Zhong H,Gong JP.Mirizzi syndrome∶Experience in diagnosis and treatment of 25 cases.Am Surg 2012;78∶61-5.
3.Shah O,Dar M,Wani M,et al.Management of Mirizzi syndrome∶A new surgical approach.ANZ J Surg 2001;71∶423-7.
4.Pemberton M,Wells AD.The Mirizzi syndrome.Postgrad Med J 1997;73∶487-90.
5.Csendes S,Diaz J,Burdiles P,et al.Mirizzi syndrome and cholecystobiliary fistula∶A unifying classification.Br J Surg 1989;76∶1139-43.
6.Chan CY,Liau KH,Ho CK,et al.Mirizzi syndrome∶A diagnostic and operative challenge.Surgeon 2003;1∶273-8.
7.Aydin U,Yazici P,Ozsan I,et al.Surgical management of Mirizzi syndrome.Turk J Gastroenterol 2008;19∶258-63.
8.England RE,Martin DF.Endoscopic management of Mirizzi's syndrome.Gut 1997;40∶272-6.
9.Antoniou SA,Antoniou GA,Makridis C.Laparoscopic treatment of Mirizzi syndrome∶A systematic review.Surg Endosc 2010;24∶33-9.
10.Wehrmann T,Riphaus A,Martchenko K,et al.Intraductal ultrasonography in the diagnosis of Mirizzi syndrome.Endoscopy 2006;38∶717-22.
11.Ahlawat SK,Singhania R,Al-Kawas FH.Mirizzi syndrome.Curr Treat Options Gastroenterol 2007;10∶102-10.
12.Salloum RM,Koniaris L.Image of the month.Mirizzi syndrome.Arch Surg 2004;139∶449-50.
13.Kaya D,Karcaaltincaba M,Akhan O,et al.MRCP diagnosis of Mirizzi syndrome in a paediatric patient∶Importance of T1-weighted gradient echo images for diagnosis.Pediatr Radiol 2006;36∶980-2.
14.Chowbey PK,Sharma A,Mann V,et al.The management of Mirizzi syndrome in the laparoscopic era.Surg Laparosc Endosc Percutan Tech 2000;10∶11-4.
15.Johnson LW,Sehon JK,Lee WC,et al.Mirizzi's syndrome∶Experience from a multi-institutional review.Am Surg 2001;67∶11-4.
16.Abou-Saif A,Al-Kawas FH.Complications of gallstone disease∶Mirizzi syndrome,cholecystocholedochal fistula,and gallstone ileus.Am J Gastroenterol 2002;97∶249-54.
17.Sharp CF,Garza RZ,Mangram AJ,et al.Partial cholecystectomy in the setting of severe inflammation is an acceptable consideration with few long-term sequelae.Am Surg 2009;75∶249-52.
18.Cui Y,Liu Y,Li Z,et al.Appraisal of diagnosis and surgical approach for Mirizzi syndrome.ANZ J Surg 2012;82∶708-13.
19.Erben Y,Benavente-Chenhalls LA,Donohue JM,et al.Diagnosis and treatment of Mirizzi syndrome∶23-year Mayo Clinic experience.J Am Coll Surg 2011;213∶114-9.
 Chinese Medical Sciences Journal2013年3期
Chinese Medical Sciences Journal2013年3期
- Chinese Medical Sciences Journal的其它文章
- Clinical Application of Loewenstein Occupational Therapy Cognitive Assessment Battery-Second Edition in Evaluating of Cognitive Function of Chinese Patients with Post-stroke Aphasia
- Relationship Between Programmed Death-ligand 1 and Clinicopathological Characteristics in Non-small Cell Lung Cancer Patients
- Assessment of Left Atrial Function by Full Volume Real-time Three-dimensional Echocardiography and Left Atrial Tracking in Essential Hypertension Patients with Different Patterns of Left Ventricular Geometric Models△
- Expression of microRNA-29b2-c Cluster is Positively Regulated by MyoD in L6 Cells△
- Effect of Timing of Tracheotomy on Clinical Outcomes:an Update Meta-analysis Including 11 Trials
- Role of Sclerostin in the Bone Loss of Postmenopausal Chinese Women with Type 2 Diabetes
