Clinical Observation on Electroacupuncture for Post-stroke Flaccid Paralysis
Zhu Xian-min, Hou Jing-yue
Henan University of Traditional Chinese Medicine, Zhengzhou 450008, China
Clinical Observation on Electroacupuncture for Post-stroke Flaccid Paralysis
Zhu Xian-min, Hou Jing-yue
Henan University of Traditional Chinese Medicine, Zhengzhou 450008, China
Objective: To observe the clinical efficacy of electroacupuncture (EA)in treating post-stroke flaccid paralysis.
Methods: Forty patients with post-stroke flaccid paralysis were randomized by the random number table into a treatment group and a control group, 20 cases in each. The treatment group was intervened by acupuncture at Jiquan (HT 1), Tianquan (PC 2), Ququan (LR 8), Yinlingquan (SP 9), and Yongquan (KI 1), and the control group was treated by acupuncture with conventional acupoint selection. Barthel index (BI) was adopted for evaluating the activities of daily living (ADL), and therapeutic efficacy was analyzed.
Results: The two groups both had marked increases of BI score after treatment. Compared to the control group after 1 treatment course and 2 treatment courses respectively, the treatment group had significant differences in BI score (P<0.01). The total effective rate was 100.0% in the treatment group versus 90.0% in the control group, and the difference was statistically significant (P<0.01).
Conclusion: EA at Jiquan (HT 1), Tianquan (PC 2), Ququan (LR 8), Yinlingquan (SP 9), Yongquan (KI 1) is an effective approach in treating post-stroke flaccid paralysis.
Acupuncture Therapy; Electroacupuncture; Stroke; Complications; Hemiplegia
Stroke is a disease severely damaging human health. Regarding the recovery from the stroke-induced paralysis, there is a famous six-stage approach developed by modern stroke-rehabilitation researchers[1]. Post-stroke flaccid paralysis should belong to the first stage, manifested by decreased muscular tension and muscle strength, transient antigravity movement or inability to do antigravity movement, and abnormally enlarged joint movement. This study adopted the related criteria of therapeutic efficacy in the modern rehabilitation science, and set up a control group treated with electroacupuncture (EA) at points from the Yangming Meridians, to systematically observe the clinical efficacy of EA in treating post-stroke flaccid paralysis. The report is now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria of Western medicine were based on theKey Diagnostic Points for Cerebrovascular Diseases[2]stipulated by the Fourth National Congress of Cerebrovascular Diseases. All patients were diagnosedwith stroke by clinical examination and CT or MRI test. The diagnostic criteria of traditional Chinese medicine were made according to theStandard for Diagnosis and Therapeutic Effect Evaluation of Stroke(Trial) developed by the Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine in 1996[3].
1.2 Inclusion criteria
In conformity with the diagnostic criteria and confirmed by CT or MRI; clinically manifested by flaccid hemiplegia; aged ≤5 years old, disease duration 2-30 d; with stable disease condition and being conscious; decreased or loss of muscular tension, belonging to the first stage of the Brunnstrom approach; initial onset or having a history of stroke but without any sequelae.
1.3 Exclusion criteria
Having a past history of motor dysfunction, or being in co-morbid with severe hypertension, coronary heart disease, pulmonary infection, kidney dysfunction, and diabetes, or psychological diseases; accompanied by agnosia or apraxia, defect of visual-field, or intelligence impairment; aged >75 years old or disease duration>30 d; with poor constitution, fear, and being easy to faint during acupuncture, or with contraindications of acupuncture treatment; receiving sedatives or muscle relaxants recently; with subarachnoid hemorrhage.
1.4 General data
Forty eligible patients were all from the in-patient departments of the First Affiliated Hospital or Rehabilitation Hospital of Henan University of Traditional Chinese Medicine. They were divided into a treatment group and a control group by random number table with a single-blinded method, 20 cases in each. There were no significant differences between the two groups in comparing data of gender, age, disease duration and disease type (P>0.05), indicating the comparability (table 1).
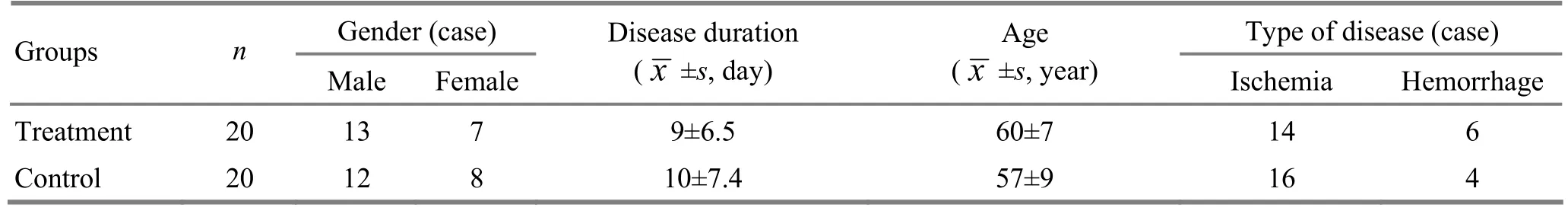
Table 1. Comparison of general data between the two groups
2 Treatment Methods
The subjects all followed the conventional interventions of internal medicine for stroke, including symptomatic and supportive treatment to monitor and regulate the risk factors of cerebrovascular diseases. In addition, they received corresponding acupuncture treatment.
2.1 Treatment group
Major acupoints: Jiquan (HT 1), Tianquan (PC 2). Ququan (LR 8), Yinlingquan (SP 9), and Yongquan (KI 1) on the affected side.
Basic adjunct acupoints: Neiguan (PC 6), Shuigou (GV 26), Sanyinjiao (SP 6), Baihui (GV 20), Sishencong (EX-HN 1), Baxie (EX-UE 9), and Bafeng (EX-LE 10).
Adjunct acupoints based on syndrome differentiation: Taichong (LR 3) and Taixi (KI 3) were added for hyperactivity of liver-yang; Fenglong (ST 40) and Hegu (LI 4) were for collaterals blocked by wind phlegm; Quchi (LI 11), Neiting (ST 44), and Fenglong (ST 40) were for excess of Fu organs due to phlegm heat; Qihai (CV 6), Xuehai (SP 10), and Zusanli (ST 36) were for blood stagnation due to qi deficiency; Taixi (KI 3) and Fengchi (GB 20) were for wind induced by yin deficiency[4].
Operation: After standard sterilization, filiform needles of 0.30 mm in diameter and 50 mm in length were selected for acupuncture. When Jiquan (HT 1) was needled, the armpit hair should be avoided. The needle was inserted for 30-45 mm, with lifting-thrusting manipulations, better to induce distending and twitching sensations to the upper limb. Tianquan (PC 2), Ququan (LR 8), Yinlingquan (SP 9), and Yongquan (KI 1) were punctured perpendicularly, with liftingthrusting manipulations to make twitching sensation. Neiguan (PC 6) was punctured perpendicularly with reducing needling techniques. Shuigou (GV 26) was punctured with bird-pecking method, better to make eyeballs moisturized. Sanyinjiao (SP 6) was punctured obliquely with an angle of 45° between the needle and the medial edge of tibia. Lifting-thrusting tonifying manipulations were conducted after needling sensation was achieved. Baihui (GV 20), Sishencong (EX-HN 1), Baxie (EX-UE 9), and Bafeng (EX-LE 10) were treated with even reinforcing-reducing manipulations. Numbdistending and twitching sensations were taken as the evaluation of acupuncture for all acupoints. Afterwards, the doctor would lift up the needles a little bit to avoid stimulating the nerve trunk directly. A pair of acupoints were selected respectively from the upper and lower limbs (the points were used alternately) to connect to G6805-2 EA apparatus, with sparse-dense wave, and intensity within the tolerance of patient. It should produce rhythmic twitching movements of muscles, stretching elbow, knee, wrist, and ankle to move,especially making the back of hand and dorsum of foot to make dorsal flexion and adduction movements. The needles were retained for 30 min. The treatment was given once per day, 6 times a week, 30 sessions as a treatment course, and 2 courses were given in total.
2.2 Control group
Major acupoints: Jianyu (LI 15), Quchi (LI 11), Shousanli (LI 10), Hegu (LI 4), Biguan (ST 31), Liangqiu (ST 34), Zusanli (ST 36), and Jiexi (ST 41) on the affected side.
Adjunct acupoints: The basic adjunctive points and the adjunctive points based on syndrome differentiation were all the same as those in the treatment group.
Operation: After standard sterilization for skin, filiform needles of 0.30 mm in diameter and 50 mm in length were used for acupuncture. After needling sensation was achieved, a pair of acupoints were selected respectively from the upper and lower limbs (the points were used alternately) to connect to G6805-2 EA apparatus. The stimulation parameters, needle-retaining time, and treatment course were all the same as those in the treatment group.
3 Therapeutic Effects Observation
3.1 Observation indexes
3.1.1 Modified Ashworth scale (MAS)
The muscular tensions of all patients were determined as 0 degree by the MAS[5]before admission to the hospital.
3.1.2 Activities of daily living (ADL)
The ADL was evaluated by using the Barthel index (BI)[6].
3.2 Criteria of therapeutic efficacy
There isn’t a universally agreed criterion of therapeutic efficacy. Therefore, Nimodipine evaluation method was adopted by consulting the involved literatures[7-9]to calculate the improvement rate of BI score.
Improvement rate of BI score = (Post-treatment BI score - Pre-treatment BI score) ÷ Pre-treatment BI score × 100%.
Markedly effective: Improvement rate of BI score≥60%.
Effective: Improvement rate of BI score ≥40%.
Improvement: Improvement rate of BI score ≥20%, but <40%.
Invalid: Improvement rate of BI score <20%.
3.3 Treatment result
3.3.1 Comparison of BI before and after treatment
After treatment, BI score increased in both groups. After 1 and 2 treatment courses respectively, the differences in BI score were statistically significant between the two groups (P<0.01), indicating that the treatment group should have a better improvement than the control group (table 2).
Table 2. Comparison of BI before and after treatment (, point)
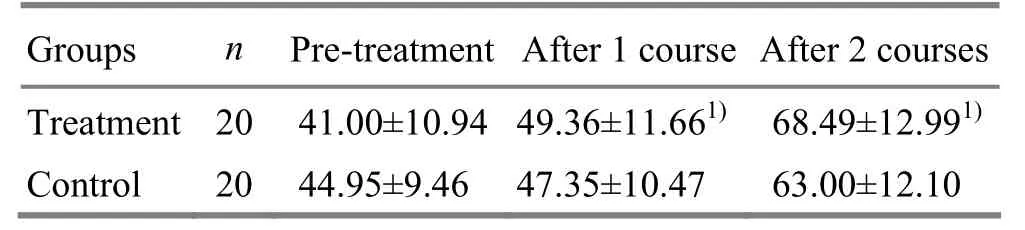
Table 2. Comparison of BI before and after treatment (, point)
Note: Compared with the control group, 1)P<0.01
Treatment2041.00±10.94 49.36±11.661)68.49±12.991)Control 2044.95±9.46 47.35±10.47 63.00±12.10
3.3.2 Comparison of therapeutic efficacy
The total effective rate was 100.0% in the treatment group versus 90.0% in the control group, and the difference was statistically significant (P<0.05), suggesting that the treatment group should have a better total effective rate than the control group (table 3).
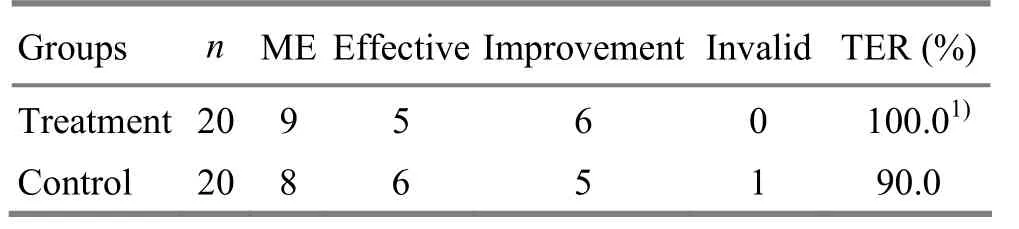
Table 3. Comparison of therapeutic efficacy (case)
4 Discussion
Flaccid paralysis during the acute stage of stroke is caused by sudden injuries of the pyramidal tract, and subsequent failure to inhibit the stretch reflex of muscles, also called flaccid stage. Generally, it will take 3 weeks to recover by itself[10]. The major acupoints chosen in the treatment group are located around limb joints, and closely related to the distribution of nerves and muscles. There are cubital nerve, median nerve, medial antebrachial cutaneous nerve, and medial brachial cutaneous nerve in the deep layer of Jiquan (HT 1); there distribute the medial brachial cutaneous nerve and musculocutaneous nerve in the deep layer of Tianquan (PC 2); there exist the medial cutaneous nerve trunk of calf and tibial nerve in the deep layer of Yinlingquan (SP 9); the saphenous nerve, obturator nerve, and tibial nerve are in the deep layer of Ququan (LR 8); Yongquan (KI 1) has the medial plantar nerve in its deep layer. By stimulating the neural cells, EA promotes the recovery of contracting and stretching functions of the involved muscles and shortens the recovery process of limb function. The sparse-intense wave is a complex wave composed of sparse wave and dense wave simultaneously and alternately. It can produce exciting-predominant effect and induce rhythmic contraction of muscles, by which, the bloodand lymph circulation and ions are regulated, nutrition metabolism is intensified, and micro-circulation is improved. The rhythmic contraction and stretching movements can increase the muscular tension and relieve the affected limbs from flaccid and numb status gradually. With the restoration of muscular tension and the increasing stability of joints, the joints can steadily regain their due movement scopes. It finally benefits the recovery of the general limb function. Clinical researches show that the sparse-dense wave and interrupted wave can avoid causing adaptation to the nerves, and the electric impulses of complex frequencies can make the muscles contract and stretch rhythmically, which can benefit the increase of the muscular tension[11]. After receiving EA treatment, the patients all gained obvious improvement revealed by electromyography (EMG) examination and sensory nerve function, and the muscle fibers also regained the innervation.
Post-stroke flaccid paralysis should be under the scope of Pian Ku, Pian Feng, or hemiplegia in traditional Chinese medicine, with wind, phlegm, and fire often seen in the excess syndrome, and qi-blood deficiency often seen in the deficiency syndrome. The flaccid stage is majorly occupied by deficiency syndrome, in co-morbid with blood stagnation due to the failure of qi to circulate blood properly. The brain houses mind and wisdom. When pathogens go up to interfere with the brain and block orifices, the brain will lose its function and limbs will be out of control. Then there appears flaccid paralysis[12-14]. Therefore, the major pathogenic factor of stroke should be blood stagnation due to qi deficiency, and the co-interference of phlegm and stagnation. In the treatment group, Jiquan (HT 1) and Tianquan (PC 2) were selected to unblock blood vessels and guarantee the sufficient heart blood to nourish the mind and improve the function of brain, and relieve the paralysis of the upper limb. Yinlingquan (SP 9) is the He-Sea acupoint of the Spleen Meridian, working to tonify the spleen and clearing dampness, supplement qi and blood, and strengthen the function of limb muscles. Ququan (LR 8) is majorly used for flaccidity and paralysis of lower limbs. Yongquan (KI 1) can nourish kidney yin, promote blood circulation and get rid of stagnation, produce marrow and benefit the brain, and promote the recovery of toe movements. The above points are used together to tonify qi and promote blood circulation, get rid of stagnation and unblock meridians and collaterals, open orifices and wake up mind. The study indicates that this point selection method has better therapeutic efficacy in treating post-stroke flaccid paralysis than selecting points only from the Yangming Meridians, and it’s worth promotion in clinic.
[1] Brunnstrom S. Movement Therapy in Hemiplegia: A Neurophysiological Approach. New York: Harper and Row Publishers, 1970: 5-15.
[2] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[3] Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine. Standard for diagnosis and therapeutic effect evaluation of stroke (trial). Beijing Zhongyiyao Daxue Xuebao, 1996, 19(1): 55-56.
[4] Shi XM. Acupuncture-moxibustion Science. 2nd Edition. Beijing: China Press of Traditional Chinese Medicine, 2007: 217.
[5] Department of Medicine of Ministry of Health of the People’s Republic of China. Diagnostic and Treatment Principles of Rehabilitation Science (First Volume). Beijing: Huaxia Publishing House, 1999: 59.
[6] Wang YJ. Progress of Modern Neurology. Beijing: Scientific and Technical Documentation Press, 1999: 53-56.
[7] Zhao JG, Xu ZH, Cao CH. Clinical study on needling Zhuiti Region in treating the spastic state of apoplectic patients. Zhongguo Zhongyiyao Xinxi Zazhi, 2003, 10(7): 10-12.
[8] Ministry of Health of the People’s Republic of China. Diagnostic and Treatment Principles of China Rehabilitation Science. Beijing: Huaxia Publishing House, 1998: 59.
[9] Miao HS, Zhu YL. Rehabilitation Evaluation and Treatment of Stroke. Beijing: Huaxia Publishing House, 1996: 9-22.
[10] Zhang ZM. Relationship between muscle tension and recovery of upper limbs motor function of stroke patients. Zhongguo Kangfu Lilun Yu Shijian, 2004, 10(6): 373-374.
[11] Zhu Q. Clinical study on electroacupuncture at nerve stimulation points for post-stroke flaccid paralysis. Shandong Zhongyiyao Daxue Xuebao, 2007, 31(6): 469-471.
[12] Zhang HM, Wu CH, Song ZB, Zhao G, Shen XH. Study on rehabilitating effect of acupuncture plus kinetotherapy for early hemiplegia. J Acupunct Tuina Sci, 2006, 4(6): 342-346.
[13] Song YL, Liu TY, Yang HY. Comparative study on exercise plus acupuncture for spastic and flaccid paralysis. Shanghai Zhenjiu Zazhi, 2010, 29(7): 478-481.
[14] Yu GQ. Observations on the efficacy of GV-regulating and Yang-activating acupuncture in treating postapoplectic spasmodic paralysis. Shanghai Zhenjiu Zazhi, 2009, 28(10): 577-578.
Translator: Hong Jue
R246.6
A
Date: April 20, 2013
Author: Zhu Xian-min, professor, master supervisor
Hou Jing-yue, M.D.
E-mail: lilamond@163.com
 Journal of Acupuncture and Tuina Science2013年4期
Journal of Acupuncture and Tuina Science2013年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Efficacy Observation on Acupuncture Combined with Auricular Point Sticking Treatment for Primary Dysmenorrhea
- Immediate Effects of Hegu Needling on Adhesive Scapulohumeral Periarthritis
- Clinical Observation on Acupoint Sticking Therapy for Lumbar Intervertebral Disc Hernination
- Clinical Study on Acupoint Injection for Primary Osteoporosis
- Effect of Electroacupuncture on Anxiety and Craving in Heroin Addicts During Detoxification
- Treatment of Post-stroke Spastic Hemiplegia by Acupuncture plus Rehabilitation Training
