Outpatient versus inpatient laparoscopic cholecystectomy: a single center clinical analysis
Wu Ji, Kai Ding, Ling-Tang Li, Dan Wang, Ning Li and Jie-Shou Li
Nanjing, China
Outpatient versus inpatient laparoscopic cholecystectomy: a single center clinical analysis
Wu Ji, Kai Ding, Ling-Tang Li, Dan Wang, Ning Li and Jie-Shou Li
Nanjing, China
(Hepatobiliary Pancreat Dis Int 2010; 9: 60-64)
laparoscopic cholecystectomy;outpatient surgery;fast-track surgery
Introduction
As laparoscopic cholecystectomy (LC) matures,and its indications expand.[1,2]Many medical centers around the world have performed outpatient laparoscopic cholecystectomy (OPLC) in recent years.[3,4]Several studies showed that OPLC has a rapid bed turnover rate and reduces total cost.[5-7]In China however OPLC has been performed because of numerous restrictions. At the well-equipped outpatient operating room of Jinling Hospital, Nanjing, from April 2007 to December 2008, we performed OPLC for 100 patients.These patients were compared with another 100 patients undergoing inpatient laparoscopic cholecystectomy (IPLC)in the same time period, attempting to evaluate the bene fi ts, feasibility, and safety of OPLC.
MethodsPatients
Hundred patients who hadundergone OPLC at our hospital were retrospectively studied, and data were categorized according to age, gender, comorbidities,preoperative diagnosis, operative indications, American Society of Anesthesiology (ASA) class, operative time,intraoperative blood loss, intraoperative and postoperative complications, postoperative time for diet intake,time of postoperative hospitalization, and post-surgical complications. Patient satisfaction with OPLC was analyzed by a grading system for postoperative followup. Another 100 patients who had undergone inpatient laparoscopic cholecystectomy were enrolled similarly into the IPLC group.
The inclusion criteria of cases in the study included clinical diagnosis with various gallbladder diseases including cholecystitis, cholelithesis, and gallbladder polyps, as well as denial of any prior abdominal surgery.A conversion was de fi ned as making any unexpected incision at the abdominal wall for the purpose of completing any portion of the laparoscopic procedure that could not, even after appropriate attempts, be accomplished laparoscopically without breaching the principles of the safety of laparoscopic procedures.
Methods
Preoperative examination of the IPLC and OPLC groups included ultrasonography, electrocardiography,chest X-ray and routine blood test, liver and renal function test. For the patients of the IPLC group, these tests were performed on their admission, whereas the OPLC patients underwent the tests in the out-patient clinic. The results of the tests were evaluated and decided by the OPLC inclusion criteria approved by the hospital ethics committee. After being selected for OPLC, the patient came to the outpatient clinic, where specialized nursing staff registered the patient, set up records,reviewed the disease-related information, and booked the operating theater for the procedure. On the day before surgery, the patient with his/her family members returned to the outpatient clinic, where they were asked to sign a consent form for the surgery after extensive discussion of the bene fi ts and risks of the procedure.Then, they prepaid the estimated costs for the surgery and possible hospital stay. On the morning of the operation day, the patient arrived at the out-patient surgery center one hour before the planned operation after fasting for more than 6 hours.
Anesthesia was induced with propofol, remifentanil,and atracurium. At this time, the patient was intubated and continuously anesthetized by inhaling anesthetics.In the induction period, a single dose of cefenradine was given intravenously for infectious prophylaxis. Intraoperatively, electrocardiography, arterial line monitoring,and blood gas analysis were continued. Laparoscopic cholecystectomy had been standardized for the patients of the OPLC and IPLC groups, and was performed in the morning in the well-equipped operating room at our out-patient clinic. In the immediate postoperative period, a 5-HT3 receptor antagonist was administered to prevent postoperative nausea and vomiting.
The patients of the OPLC group were sent to the postoperative anesthesia care unit (PACU) for extubation and immediate postoperative care. Twelve hours after the surgery. Both surgeons and anesthetists jointly evaluated if the patients could be discharged when the following were satis fi ed:[8]1) vital signs stable for more than 4 hours; 2) appropriate awakeness, alertness, and orientation to people, place and time; 3) independent dressing and walking; and 4) no nausea, vomiting, severe pain, and incision bleeding. The criteria for admission to the surgical ward for continuous inpatient care included: 1) fl uctuating vital signs in the postoperative period; 2) incompletely resolved symptoms of nausea,vomiting and pain; 3) a signi fi cant amount of fl uid from the abdominal drain; and 4) patients and their family members who expressed a strong wish to stay in hospital.The patients discharged on the fi rst postoperative day were requested to contact the hospital shortly after arrival at home, and 24 hours after the discharge. The patients were evaluated at least once by the nursing staff.They could also consult surgeons and their associates via the internet at all times regarding any issue related to the surgery and postoperative care. The patients hospitalized were further observed, and reassessed by the surgeons for possible discharge on the second postoperative day.
The patients of the IPLC group were admitted to the surgical wards for postoperative management after immediate postoperative care. Normally, they were discharged 2-4 days after operation if no major and severe complications occurred.
In this retrospective study, the completion rate of laparoscopic cholecystectomy, operative time, estimated amount of intraoperative bleeding, time to take liquid and soft diet after operation, operative complications,length of postoperative hospital stay, and total cost for both operation and hospitalization were collected from our patient database. Satisfaction with the surgery and postoperative management was graded by patients two weeks after operation who were telephone-interviewed by nurses using a questionnaire containing 10 items with a score of 1 to 10.
In this study, SPSS 13.0 statistical software was used to establish the database for analysis. Comparison between the OPLC and IPLC groups was made with Student's t test for categorical variables. Statistical signi fi cance was de fi ned as P<0.05.
Results
In the IPLC group, LC was performed successfully for 99 patients, one of whom later changed to have an open procedure. The median operating time was 24.0 minutes and the intraoperative bleeding was estimated to be 16.2 ml. An abdominal draining tube was placed in 3 patients, in whom two tubes were removed on the fi rst day after the surgery, while the remaining one was kept until the second day. After operation, the median time to resume liquid and soft diet was 10.7 and 22.0 hours,respectively. The mean postoperative hospital stay was 58.2 hours. One patient developed a urinary infection,and recovered without any intervention. The mean total cost was 8770.5 RMB yuan. During the followup visit in the second week after operation, 19 patients graded their satisfaction with the IPLC management at 10, and 71 patients gave 6 to 9. However, 10 patients were dissatis fi ed with the IPLC pathway, giving scores less than 6. Taken together, the satisfaction rate was 90% (Table).
In the OPLC group, the completion rate for LC was 99% with one patient who had the operation converted.The median operative time was 21.6 minutes, and intraoperative blood loss was about 14.7 ml. Drainage tubes were used in 2 patients: one tube removed on the fi rst day and the other taken out on the second day after the operation. The median time to have clear liquid was 11.3 hours and a semi-liquid diet was 20.1 hours after the operation. The mean time for postoperative hospital observation was 28.5 hours in two patients with umbilical infection and subhepatic abscess which were resolved after conservative treatment. On the fi rst postoperative day, 89 patients were discharged home while 11 were hospitalized for further observation. Of the 11 patients, 6 had uncontrolled pain, 2 manifested signi fi cant nausea and vomiting, and 1 reported blurred vision. The remaining 2 patients did not wish to leave the hospital even though their condition was stable enough for discharge. All the 11 patients went home on the second day. There were no readmissions in the OPLC group. The total cost for both surgery and hospital stay was 7235.7 RMB yuan. Followup was conducted two weeks after the surgery. Thirtyone patients were well satis fi ed and 63 were satis fi ed, but 6 were dissatis fi ed with the OPLC management. Therefore,for the OPLC group, the satisfaction rate was 94% withfour patients complaining of pain and vomiting on the fi rst day at home, but the other two patients gave no speci fi c reasons (Table).
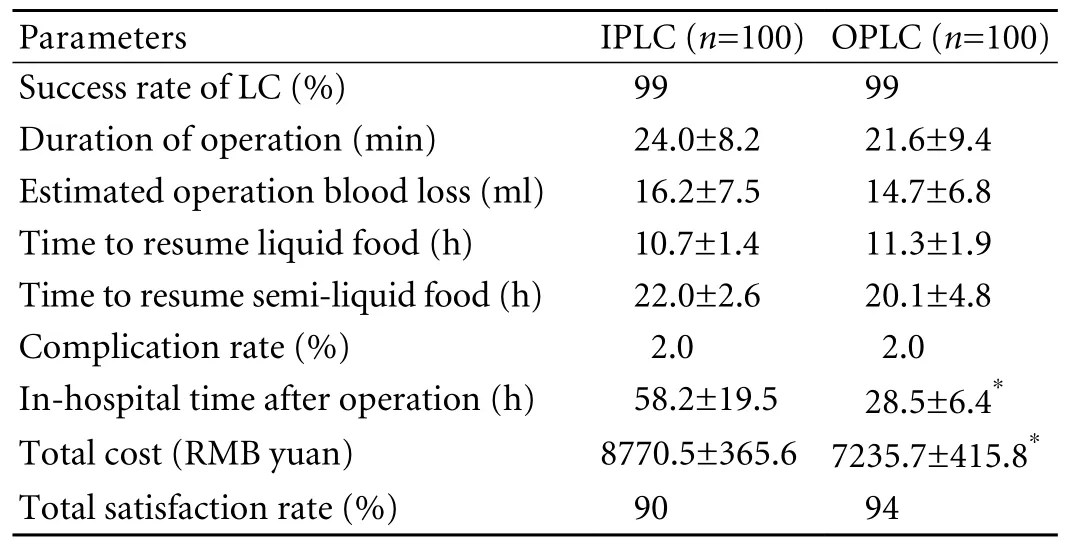
Table. Comparison of perioperative parameters between the IPLC and OPLC groups
Discussion
The practice of OPLC was conceptized in the early 1990s. It has been shown that OPLC shortens hospital stay, and substantially lowers medical costs.[9]Studies reported that OPLC accounted for 60%-90% of LCs in several centers, and most patients were safely discharged from hospitals after 6-8 hours of postoperative observation.[10,11]Besides the OPLC management was widely accepted by patients and their families. However, large randomized prospective studies are not available to further con fi rm the safety, feasibility, cost-effectiveness,and patient satisfaction of OPLC.
Our study did not show signi fi cant differences between OPLC and IPLC in success rate, operative time, blood loss during surgery, time to resume liquid and semi-liquid diet, complication rate, and patient satisfaction rate. This fi nding indicates that OPLC is feasible, safe, and can be accepted by patients. The safety of OPLC management can be guaranteed by several factors such as strict selection criteria, thorough preoperative preparation, and experienced laparoscopic surgeons, especially careful monitoring and examination with prompt intervention in the PACU and postoperative holding unit, which could be the key to ensuring the success of OPLC. It has been shown that the major risk in OPLC management is early postoperative complications such as intra-abdominal hemorrhage, bile leakage, vascular injury, or subcutaneous emphysema of the neck and chest. However, our experience showed that the risk can be found by careful observation from 12 to 24 hours after the operation, and if treated early the management plan was not compromised.
We adopt the one-day OPLC management described in several reports that patients are scheduled for LC in the morning,[12,13]then observed in the postoperative holding room in the outpatient surgical unit for close monitoring of vital signs and other postoperative symptoms. On the fi rst postoperative morning, if the patients tolerate a liquid diet without any adverse effect,they could be discharged from the hospital.[14]We believe this management not only ensures the safety of patient care,but also compensates for the traditional concepts of Chinese people on postoperative inhospital management.
Other interesting fi ndings of our study include the signi fi cant differences between the OPLC and IPLC groups in the length of postoperative hospitalization and the total expenses for surgery and hospital stay. These results re fl ect the advantages of the OPLC management.OPLC can: 1) shorten postoperative hospital stay and waiting time for surgery, indicating that OPLC management fi nancially bene fi ts both patients and hospitals by facilitating in-patient bed turnover and saving medical costs; 2) liberate patients early from the discomfort of hospitalization; 3) decrease the chance of nosocomial infections; and 4) allow patients to follow their own schedules for preoperative examinations and surgery,thereby ensuring a personalized management. Moreover,this fast-track surgery can hasten postoperative recovery and subsequently accelerates the patients' return to work and a normal life.
Medical expenses have always been a major issue in every health care system worldwide. It has been reported that OPLC lowers medical care costs by 20%-40%those for inpatient LC.[15]In our study, the total cost for OPLC decreased by 17.5% compared with that for IPLC.Although the cost reduction in our study is less than the reported, it is still signi fi cant for the current healthcare system in China, where the overwhelming numbers of patients have limited access to the healthcare resources.
OPLC management also has several disadvantages: 1)restricted indications, i.e., many patients are not selected for OPLC, especially in the mainland of China; 2) high resource rquirements, like a well-equipped operation room and well-trained surgical team, which prevent many hospitals from OPLC practice; in addition, OPLC requires surgeons being capable of performing LC and having experienced laparoscopic skills; 3) heavy work load and psychological tolerance for patients and their family members; 4) lack of supporting management of post-hospital discomfort such as pain, nausea and vomiting, which will eventually result in dissatisfaction with OPLC. More importantly, hospitals and surgeons must bear great liability for any postoperative complications that cannot be identi fi ed and managed properly.
OPLC practice originated in the United States and other developed countries. However this practice has not been widely accepted in China. First, the costs covering surgery and hospitalization are only at a low proportion of the total costs, so the superiority of OPLC did not decrease medical expenses and save medical resources in China. Second, imperfect medical and surgical facilities might nullify the safety of OPLC. Third, the practice of OPLC has not been appropriately appreciated by medical institutes, medical staff, patients and families, and the quality of post-hospital patient care has been questioned by patients and their family members. Most importantly,the underdeveloped medical insurance system cannot satisfy the requirements of OPLC. Currently OPLC is still not listed in medical insurance coverage. Last,insuf fi cient community healthcare services may not be prompt enough to manage postoperative complications in the post-hospital phase. Therefore, OPLC may not be widely practiced in China until these issues have been solved[16,17]The practice of OPLC is an outcome of the global development of medical technology, health care and medical services, insurance systems, and the social environment.
Laparoscopic cholecystectomy has dramatically transformed the management of gallbladder pathology in the past decades, and had a major in fl uence on patient management in the development of modern surgery. The practice of OPLC has further enhanced this in fl uence,hence it may soon become the new "gold standard" for the management of gallbladder disease.[18,19]Currently,although OPLC is not widely practiced in China, with its advantages and bene fi ts, and more importantly, its match with the direction of current medical reform in China,OPLC will be extensively accepted by surgeons and patients in the near future.[20]We suggest OPLC should be performed in some tertiary hospitals with well-trained staff and well-equipped outpatient surgery facilities,then gradually introduced to other lower level hospitals and medical centers. With the success of the practice of OPLC, the underlying principles may be applied to other practices such as general surgery, gynecology, and urinary surgery.
Funding: This study was supported by a grant from the Special Purpose Fund of the Medical Science Project of the PLA (08Z007).Ethical approval: Not needed.
Contributors: LJS proposed the study and wrote the fi rst draft.JW analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. LJS is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Ji W, Li LT, Li JS. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int 2006;5:584-589.
2 Ji W, Li LT, Wang ZM, Quan ZF, Chen XR, Li JS. A randomized controlled trial of laparoscopic versus open cholecystectomy in patients with cirrhotic portal hypertension. World J Gastroenterol 2005;11:2513-2517.
3 Chauhan A, Mehrotra M, Bhatia PK, Baj B, Gupta AK. Day care laparoscopic cholecystectomy: a feasibility study in a public health service hospital in a developing country. World J Surg 2006;30:1690-1697.
4 Topal B, Peeters G, Verbert A, Penninckx F. Outpatient laparoscopic cholecystectomy: clinical pathway implementation is ef fi cient and cost effective and increases hospital bed capacity.Surg Endosc 2007;21:1142-1146.
5 Basu S, Giri PS, Roy D. Feasibility of same day discharge after mini-laparotomy cholecystectomy--a simulation study in a rural teaching hospital. Can J Rural Med 2006;11:93-98.
6 Gurusamy K, Junnarkar S, Farouk M, Davidson BR. Metaanalysis of randomized controlled trials on the safety and effectiveness of day-case laparoscopic cholecystectomy. Br J Surg 2008;95:161-168.
7 Seim AR, Andersen B, Berger DL, Sokal SM, Sandberg WS. The effect of direct-from-recovery room discharge of laparoscopic cholecystectomy patients on recovery room workload. Surg Innov 2006;13:257-264.
8 Psaila J, Agrawal S, Fountain U, Whit fi eld T, Murgatroyd B,Dunsire MF, et al. Day-surgery laparoscopic cholecystectomy:factors in fl uencing same-day discharge. World J Surg 2008;32:76-81.
9 Paquette IM, Smink D, Finlayson SR. Outpatient cholecystectomy at hospitals versus freestanding ambulatory surgical centers. J Am Coll Surg 2008;206:301-305.
10 Parvaiz MA, Hafeez R. Randomized clinical trial of day-care versus overnight-stay laparoscopic cholecystectomy. Br J Surg 2006;93:639-640.
11 Kasem A, Paix A, Grandy-Smith S, El-Hasani S. Is laparoscopic cholecystectomy safe and acceptable as a day case procedure? J Laparoendosc Adv Surg Tech A 2006;16:365-368.
12 Victorzon M, Tolonen P, Vuorialho T. Day-case laparoscopic cholecystectomy: treatment of choice for selected patients?Surg Endosc 2007;21:70-73.
13 Metcalfe MS, Mullin EJ, Maddern GJ. Relaxation of the criteria for day surgery laparoscopic cholecystectomy. ANZ J Surg 2006;76:142-144.
14 Barthelsson C, Anderberg B, Ramel S, Bjorvell C, Giesecke K, Nordstrom G. Outpatient versus inpatient laparoscopic cholecystectomy: a prospective randomized study of symptom occurrence, symptom distress and general state of health during the fi rst post-operative week. J Eval Clin Pract 2008;14:577-584.
15 Jain PK, Hayden JD, Sedman PC, Royston CM, O'Boyle CJ. A prospective study of ambulatory laparoscopic cholecystectomy:training economic, and patient bene fi ts. Surg Endosc 2005;19:1082-1085.
16 Skattum J, Edwin B, Trondsen E, Mjaland O, Raede J, Buanes T.Outpatient laparoscopic surgery: feasibility and consequences for education and health care costs. Surg Endosc 2004;18:796-801.
17 Mitchell M. Nursing intervention for day-case laparoscopic cholecystectomy. Nurs Stand 2007;22:35-41.
18 Bueno Lledó J, Planells Roig M, Arnau Bertomeu C, Sanahuja Santafé A, Oviedo Bravo M, García Espinosa R, et al.Outpatient laparoscopic cholecystectomy: a new gold standard for cholecystectomy. Rev Esp Enferm Dig 2006;98:14-24.
19 Ahmad NZ, Byrnes G, Naqvi SA. A meta-analysis of ambulatory versus inpatient laparoscopic cholecystectomy. Surg Endosc 2008;22:1928-1934.
20 Lammert F, Miquel JF. Gallstone disease: from genes to evidence-based therapy. J Hepatol 2008;48:S124-135.
BACKGROUND: Outpatient laparoscopic cholecystectomy(OPLC) developed in the United States and other developed countries as one of the fast-track surgeries performed in ambulatory centers. However, this practice has not been installed as a routine practice in the major general hospitals and medical centers in China. We designed this case-control study to evaluate the feasibility, bene fi ts, and safety of OPLC.METHODS: Two hundred patients who had
laparoscopic cholecystectomy for various benign gallbladder pathologies from April 2007 to December 2008 at Jinling Hospital of Nanjing University School of Medicine were classi fi ed into two groups: OPLC group (100 patients), and control group (100), who were designated for inpatient laparoscopic cholecystectomy (IPLC). Data were collected for age, gender, indications for surgery, American Society of Anesthesiology (ASA) class, operative time, blood loss during surgery, length of hospitalization, and intra- and post-operative complications. The expenses of surgery and in-hospital care were calculated and analyzed. The operative procedures and instrumentation were standardized for laparoscopic cholecystectomy, and the procedures were performed by two attending surgeons specialized in laparoscopic surgery.OPLC was selected according to the standard criteria developed by surgeons in our hospital after review. Reasons for conversion from laparoscopic to open cholecystectomy were recorded and documented.
RESULTS: One hundred patients underwent IPLC following the selection criteria for the procedure, and 99% completed the procedure. The median operative time for IPLC was 24.0
minutes, blood loss was 16.2 ml, and the time for resuming liquid then soft diet was 10.7 hours and 22.0 hours, respectively.Only one patient had postoperative urinary infection. The mean hospital stay for IPLC was 58.2 hours, and the cost for surgery and hospitalization was 8770.5 RMB yuan on average. Followup showed that 90% of the patients were satis fi ed with the procedure. In the OPLC group, 99% of the patients underwent the procedure with a median operative time of 21.6 minutes and bleeding of 14.7 ml. The patients took liquid 11.3 hours then soft diet 20.1 hours after surgery. The mean postoperative hospital stay was 28.5 hours. In this group, 89% of the patients were discharged within the fi rst 24 hours, and the remaining 11% were released within 48 hours after surgery. Two patients developed local complications. The cost for surgery and hospitalization was 7235.7 RMB yuan, which was 17.5% less than that in the IPLC group. At follow-up, 94% of the patients were satis fi ed with the surgery and short hospital stay.
CONCLUSIONS: OPLC can effectively treat a variety of benign,non-acute gallbladder diseases with shortened waiting time and postoperative hospital stay. OPLC bene fi ts the hospital with a rapid bed turnover rate, and reduces cost for surgery and hospitalization.
Author Af fi liations: Research Institute of General Surgery, Jinling Hospital,Nanjing University School of Medicine, Nanjing 210002, China (Ji W, Ding K, Li LT, Wang D, Li N and Li JS)
Jie-Shou Li, MD, PhD, Research Institute of General Surgery, Jinling Hospital, Nanjing University School of Medicine,Nanjing 210002, China (Tel: 86-25-84826808; Fax: 86-25-84803956; Email:fengboxiao@hotmail.com)
? 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
August 24, 2009
Accepted after revision December 22, 2009
 Hepatobiliary & Pancreatic Diseases International2010年1期
Hepatobiliary & Pancreatic Diseases International2010年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Critical fl icker frequency for diagnosis and assessment of recovery from minimal hepatic encephalopathy in patients with cirrhosis
- Risk factors for early recurrence of smallhepatocellular carcinoma after curative resection
- Pathological changes at early stage of multiple organ injury in a rat model of severe acute pancreatitis
- Potential etiopathogenesis of seventh day syndrome following living donor liver transplantation: ischemia of the graft?
- Comparatively lower postoperative hepatolithiasis risk with hepaticocholedochostomy versus hepaticojejunostomy
- Effect of sodium salicylate on oxidative stress and insulin resistance induced by free fatty acids
